Lameness originating from tendon sheathes.
Lisa A. Fortier, DVM, PhD, Diplomate ACVS Cornell University, Ithaca, New York, USA
Laf4@cornell.edu
(Below is cut and pasted from Dr. Fortier’s “Lameness Originating from Tendon Sheaths”)
The most commonly affected tendon sheathes associated with lameness is horses are the digital, carpal, and tarsal sheaths. In general, the diagnoses of lameness originating from tendon sheathes is increasing with awareness and with the more common use of MRI. Clinical signs associated with tendon sheath lameness are variable with respect to degree of lameness and extent of synovial distension. In general, the lameness will worsen with flexion and with work, but the degree of lameness is not directly associated with prognosis for return to athletic performance.
Lameness associated with the digital sheath
Lameness can be localized to the digital sheath with a low 4-point block or intrathecal anesthesia. If sepsis is suspected, a clean (non blood-contaminated) synovial fluid sample can be obtained at the base of the sesamoid bones and axial to the palmar digital neurovascular bundle.
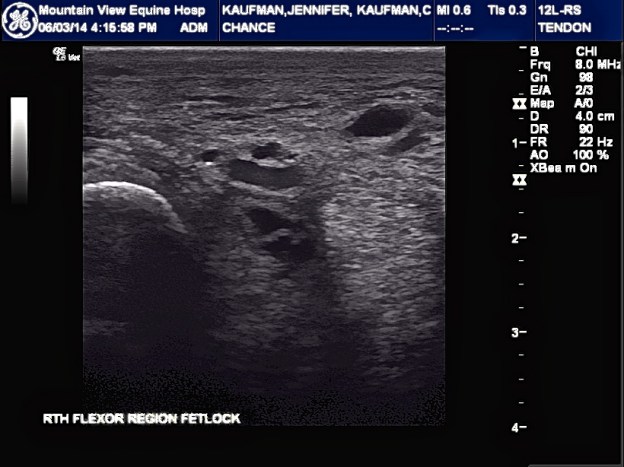
Simple annular ligament constriction, without involvement of the superficial (SDFT) or deep digital flexor tendons (DDFT) is a common cause of lameness associated with the digital sheath. When viewed from the side, the palmar/plantar profile of the digital sheath will have a “notched” or “cut-in” appearance at the fetlock joint. The integrity of the annular ligament (thickness and structure) should be evaluated using ultrasonography to be sure there are no other structures involved such as the SDFT or DDFT. Horses can be treated with intrathecal hyaluronic acid with variable success prior to surgical intervention. If the annular ligament is the sole structure involved and there are no adhesions within the tendon sheath, then a closed or semi-open annular ligament transection could be performed rather than a tenoscopic transection. If ultrasound examination reveals adhesions or synovial masses within the sheath, then tenoscopic exploration and removal of the masses/adhesions is warranted.
Performing surgical maneuvers or exploratory surgery under tenoscopic guidance has distinct advantages as compared to open approaches. Tenoscopy allows for more complete examination of the entire tendon and tendon sheath, resulting in a more accurate diagnosis than can be provided by ultrasonography and the surgeon has an opportunity for removal of pathologic tissues such as synovial proliferative masses, hyperplasic synovial tissue, and adhesions. Additionally, the use of tenoscopic portals instead of an open approach reduces potential iatrogenic damage to neighboring structures and decreases the incidence of postoperative synovial fistulation. The biggest take-home message of these notes should be that the presence or extent of synovial masses/adhesions is not directly correlated with prognosis and many horses return to full athletic performance after tenoscopic surgery and removal of adhesions/masses and annular ligament transection.
Longitudinal tears in deep flexor tendon are increasing commonly diagnosed. Like adhesions and masses, tears are frequently worse on tenoscopic exam than on ultrasound. In these cases, the tendon tear appears to be the primary cause of the tenosynovitis and the annular ligament constriction is likely secondary. Currently, debriding the tendon edges is the only treatment, but some tendon repair technique seems warranted. Ian Wright described a combined approach to repair these tears, but has subsequently discontinued this practice and simple debridement of the granulation tissue between tendon edges is recommended.