Wobblers, EPM, & Other Neurological Disorders Journal/Conference Below:
Tag Archives: epm
EPM Diagnosis and Treatment Via Acupuncture
EPM or Another Neurological Disease?
Below is an article about differentiating between EPM or other neurological disorders.
4 Horses Die Due to EPM Treatment
4 Horses Die After Receiving Compounded EPM Drug
Adverse events were reported in two Kentucky horses and eight Florida horses that received a pyrimethamine-toltrazuril combination.
BY VETERINARY PRACTICE NEWS EDITORS
Adverse events such as seizures, fever and death were reported in two Kentucky horses and eight Florida horses that received a pyrimethamine-toltrazuril combination. Four of the horses died or were euthanized and six horses are recovering, FDA reported.The U.S. Food and Drug Administration on Thursday issued an advisory about compounded veterinary medications after four horses being treated for equine protozoal myeloencephalitis (EPM) died.
Wickliffe Veterinary Pharmacy of Lexington, Ky., compounded two lots—one paste and one oral suspension—containing pyrimethamine and toltrazuril.
“At this time, FDA testing indicates that one lot of product contained higher levels of pyrimethamine than the labeling indicates,” the agency stated.
“All of the products in these lots are accounted for and are no longer in distribution,” FDA added.
The usual dose of pyrimethamine in horses is 1 mg/kg when combined with sulfadiazine as an FDA-approved treatment for EPM.
Toltrazuril is not approved for use in horses, the agency noted. Bayer Animal Health offers toltrazuril as the active ingredient in Baycox, an approved anticoccidial parasiticide used with poultry, piglets and cattle.
“In general, FDA has serious concerns about unapproved animal drugs, including certain compounded animal drugs,” the agency reported. “These drugs are not evaluated by FDA and may not meet FDA’s strict standards for safety and effectiveness.”
Drugs approved for the treatment of EPM, a neurological disease caused by a protozoal infection, include ponazuril, diclazuril and the pyrimethamine-sulfadiazine combination.
Wickliffe Response
Wickliffe Veterinary Pharmacy, a high-quality provider of customized medicinal solutions for veterinarians, is working cooperatively with federal health officials to learn more about the cause of the adverse events involving horses that received a compounded product from the pharmacy. We wish to extend our deepest sympathies to the owners of, and equine professionals associated with, the horses that have died or been euthanized.
The medication prepared by Wickliffe was specifically made for and dispensed to the horses for which the medication was prescribed. No other animal patients received the prescribed medication in question. The FDA has confirmed that all of the preparations are accounted for and secured. Accordingly, any risk of further adverse effects has been eliminated. There is no indication that any other products prepared by the pharmacy are unsafe in any way.
Wickliffe adheres to the highest safety and quality standards of the compounding pharmacy profession and follows all applicable state and federal guidelines. The pharmacy has a strong reputation and extensive history of providing excellent preparations to the equine industry. Wickliffe pledges its full dedication to ensuring the quality of its procedures.
Previous: Tips for Better Equine Radiographs
Want more Veterinary Practice news? Go here.

Another Try
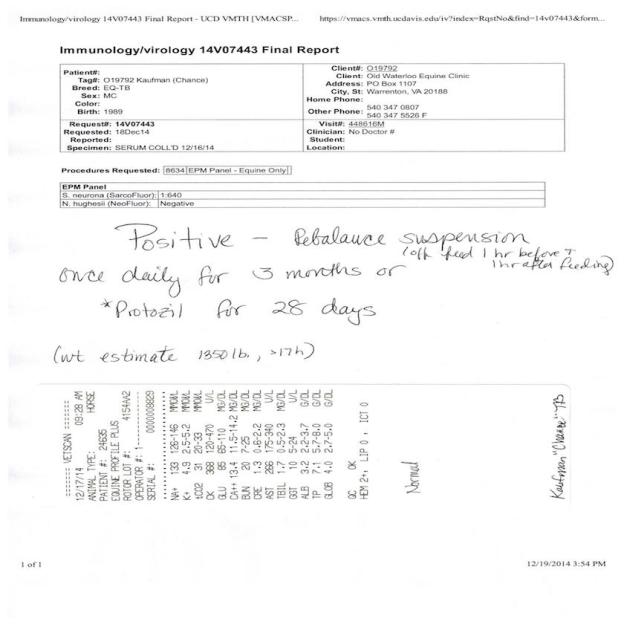
Yesterday, while at the farm, Chance’s medications arrived at my house instead of the farm. I drove home, grabbed the meds, and began my drive back to the farm. A winter storm was just beginning. 4 hours later, I dropped off the medication and turned back around to head home.
Thankfully, Chance began his second round of EPM treatment this morning.
I decided to try a different type of treatment this time around- round one: Protazil and round two: Marquis. Marquis has been around longer and has similar potential side effects and outcomes as Protazil.
Rebalance recently was linked to the death of 4 horses in 2014.
Or
Oraquin-10 which is a 10 day treatment that is more cost effective. However, it is a newer medication and the vets that I have spoken to were not as comfortable with the outcomes in the horses with EPM.
EPM Treatment Research
Ohio State University
College of Veterinary Medicine
Treatment
Several regimens have been described previously for the treatment of EPM and >60% of horses respond to treament, and that clinical signs completely regress in 55-60% of the cases. The treatment most commonly used employs a combination of potentiated sulphonamides (Trimethoprim/Sulfas) and pyrimethamine. This combination causes a sequential blockade of folate metabolism in apicomplexan protozoa. Based on a recent pharmacokinetic study of pyrimethamine in horses, the dose required to reach the minimum inhibitory concentration (MIC) for Toxoplasma gondii in CSF is 1.0 mg/kg. The recommended dose of pyrimethamine is 1 mg/kg once a day for 60 to 90 days. However, it has been suggested that high dose pyramethamine therapy over this extended time period can result in anemia. Previous work using the 1 mg/kg dose of pyrimethamine once daily did not result in anemia, but the drug was only administered for 10 days to these normal horses. The trimethoprim/sulfa combinations have been recommended at a dose of 15 to 20 mg/kg bid per os for the full treatment period. If sulfonamides are used without the trimethoprim, the dose recommended is 20 mg/kg per os once or twice per day. Most of the treatments are administered for at least 12 weeks, but must sometimes be extended to 16 weeks or more. After initial therapy has been completed, some clinicians recommend periodically placing horses back on treatment if animals undergo some unusual stress. Other intermittent treatment therapies have also been used, such as treatment once every two to four weeks, or daily during the first week of every month. Intermittent treatment may increase the risk that parasites infecting a horse develop drug resistance. Therefore, we do not recommend intermittent or periodic treatments. Recent problems with the response to current therapy has led to increasing the dose of the sulfa/pyrimethamine mixture. Earlier, the only product applied at an increased dosage was the pyrimethamine; it was administered at 1.5 mg/kg, and sometimes even 2.0 mg/kg once a day. These increased dosages were used in cases that appeared to not respond within the first 30 to 60 days. A practice currently used by some clinicians for horses that do not respond to 30 days of treatment is to increase medication dosages. For example, if using the mixture from Mortar & Pestle, the dose for a 1,000 lb. horse is 30cc. Some clinicians are increasing it to 45cc. If no response is seen after 30 days of this dosage, the amount given is further increased to 60cc per day. This should only be done in consultation with your regular veterinarian. This also increases the importance of monitoring for signs of folic acid deficiency by evaluating CBC’s at least every two weeks. Recent discussions concerning EPM have led to reports of using tetracyclines in some cases that continue to be CSF+ even after many months (six months or longer) with the sulfa/pyrimethamine combination. This use is based upon tetracycline’s inhibitory effect on protein synthesis, however, no controlled trials have been performed at this time. The only reported antiprotozoal use of tetracycline was documented in sheep which received 30 mg/kg to treat a differentSarcocystis spp. infection. This an extremely high dosage, and is not recommended for use in horses. Some clinicians have experimented with administration of 6.6 mg/kg once or twice daily for one week. It is not clear why using tetracycline, a bacteriostatic agent, for one week would be curative. We would recommend that this therapy not be used or used with extreme caution until controlled clinical trials have been completed. Additional therapies are also being used by some clinicians. These therapies include the use of immune stimulants such as Eqstim, Equimune, alpha-interferon, or levamisole. These compounds may boost non-specific cell-mediated immunity. Cell-mediated immunity is necessary to rid the body of these parasites. The efficacy of these compounds has been established in humans with leishmaniasis. A new therapy (Diclazuril) has been receiving a lot of press recently and has been under study by the University of Kentucky. This new compound is a triazine derivative that has been used as a coccidiostat in other countries for a number of years. The site at which these compounds exert their effect is called a chloroplast which do not exist in mammals. For this reason, the compound should not be toxic to mammals, however, the toxicity studies have not been completed to date. The efficacy of this compound is very similar to the standard therapy discussed above, however, the treatment period is much shorter (four weeks) and therefore less costly. This compound has been used primarily in horses that have relapsed after the standard therapy with reasonably good success. This compound is available through the AAEP and the FDA by special permit. An additional triazine derivative (Toltrazuril) is available through the same sources as the Diclazuril. Current clinical trials are being performed at several sites throughout the US to establish efficacy against Sarcocystis neurona. A new therapy called Nitazoxanide (NTZ) is being investigated by Blue Ridge Pharmaceuticals. NTZ is a thiazolide derivative that demonstrates a wide spectrum of activity against bacteria, protozoa, and intestinal helminths. The drug is in development for humans to treat parasitic infections that are common in developing countries and to treat immunocompromised patients afflicted with cryptosporidiosis. Veterinarians may obtain more details on NTZ. The area is password protected. Please call 800-870-4264 to obtain the password to enter this area. We will need your name, your clinic address, your state veterinary license number, and your DEA number. When the horse has an acute onset of EPM which results in dramatic and progressive clinical signs, the use of antiinflammatory medications has been recommended. Use of antiinflammatory medications such as banamine phenylbutazone may be helpful. Intravenous administration of medical grade dimethyl sulfoxide (DMSO) at a dose of 1.0 ml/kg (approximately 1 gm/kg) in a 10% solution once daily for three days in a row. Some clinicians use dexamethasone parenterally in severely affected horses at a dose rate of 0.05 mg/kg bid or sometimes empirically at 50 mg. bid. However, we believe corticosteroids should be used judiciously. The exacerbation of signs in stressed patients and reports of horses with EPM showing a worsening of signs following the use of these medications suggest immunosuppression should be avoided. Ancillary treatments may include padded helmets, slings, good supportive care and a deeply bedded stall.Many horses appear to relapse days, weeks or months after treatment has stopped. Some apicomplexans have latent stages, however, Sarcocystis spp. are not known for this phenomenon. Sarcocystis faculata encephalitis in birds may persist for several months without reinfection, but this phenomenon may simply represent a low level infection and not the development of a true latent parasitic stage. A great deal concerning the life cycle of coccidia remains unknown. Now with the ability to produce experimental infections, we may be able to determine if S. neurona forms a latent stage or maintains a persistent, low level foci of infection. Re-infection may also be responsible in some cases. Reports at the EPM workshop in March of 1996 indicate that relapses occur approximately 10% of the time. More recently, it has been suggested that the relapse rate may be as high as 28%. However, this may be compounded by the premature withdrawal of medication or irregularities during medication administration. The efficacy of preventive therapies is open to debate.Because of the suspicion that protozoal infections occur more commonly in immunocompromised patients, immunomodulators or other therapies which may have a non-specific enhancement of the immune system may be helpful. The use of these products may have merit but further investigation is necessary. It is possible that these drugs may also enhance the immunopathologic effects associated with CNS infection.Prolonged therapy with antifolate medications should be monitored for signs of bone marrow suppression with resultant anemia, thrombocytopenia and/or neutropenia. Frequent blood samples for CBC’s is suggested on a biweekly basis. All horses that are receiving antifolate medications should have their blood tested for folate levels on a monthly basis. Antifolate medications may also cause reduced spermatogenesis in stallions and may be teratogenic to the fetus in mares. There is evidence to suggest that combinations of pyrimethamine and folic acid in the pregnant animal may lead to congenital defects in the fetus. This has been demonstrated in humans, rats, mice, hampsters, and pigs. There is also some evidence to suggest that this also happens in horses, therefore, we do not recommend the use of folic acid supplementation in horses, particularly in pregnant mares. The authors also recommend supplementation with vitamin E at the rate of 8,000 to 9,000 IU per day. Due to the role of vitamin E as an antioxidant, we feel that adding this to the treatment may aid in the healing of the nervous tissue. Acute colitis has also been associated with use of trimethoprim/sulfa combinations.It appears with the increased dosage of pyrimethamine that is being utilized for today’s treatment of EPM as well as the experimental medication usage, there is an increased incidence of what some people term a “treatment crisis”. This is a real problem that is a concern for many clinicians. It would appear this is related to a large dose of medication and subsequent development of an inflammatory response to the killing of large numbers of parasite at one time. The spinal canal is a very narrow space with limited room for expansion due to inflammation. Therefore it would seem prudent to start horses on EPM treatment with NSAID therapy at the same time to reduce inflammation and perhaps prevent this so-called crisis.
Merck Manual Treatment The FDA-approved treatments for EPM are ponazuril (5 mg/kg/day, PO, for 28 days), diclazuril (1 mg/kg/day, PO, for 28 days), and a combination of sulfadiazine and pyrimethamine (20 mg/kg and 1 mg/kg, respectively, for at least 90 days). The bioavailabilities of ponazuril and diclazuril are improved by concurrent PO administration of corn oil or DMSO. A loading dose of ponazuril (15 mg/kg, PO) may be given on the first day of treatment to rapidly attain therapeutic blood levels. The sulfadiazine/pyrimethamine product must be given at least 1 hr before or after hay is fed. Anemia may develop after prolonged treatment with sulfadiazine/pyrimethamine and is best prevented by providing folate-rich green forage such as alfalfa hay or green pasture. Approximately 60% of horses improve wit each type of treatment, but <25% recover completely. Relapses occur commonly up to 2 yr after discontinuation of antiprotozoal therapy. Because immunosuppression/immunodeficiency may be a risk factor for EPM, immunomodulators (eg, mycobacterial cell-wall derivative, levamisole, killed parapox ovis, or transfer factor) are sometimes given as ancillary therapy.
Where to go from here…
Over the last couple weeks, I have seen moments where C looks like a healthy 8 year old, who can do anything, and other days, he looks like he did when we began treatment for EPM. The entire journey is daunting and heart wrenching…but how can I give up hope when, according to the numerous veterinarians and the countless journals, he is not in pain? And when his eyes light up when he sees me? And when he rolls around in the snow? Or is laying in the sunshine? Or when he gobbles up his food? Or when I see him close his eyes and hear him let out a sign while I groom him? Or hear him whinny? Or run around in the field? I can’t. I won’t. Not after the 15 years he gave me- doing the work, moving with me, being my buddy. I owe him. So, the endless hours of research will continue, as it has with each hurdle over the many months. Fingers crossed.

A Month Later
Luckily, after about one week of stall rest and hand walking, along with a stronger anti-inflammatory, Chance has begun to show improvements over the last couple weeks of treatment.
Chance has almost completed his first 30 days of EPM treatment and has about a day or so left of the Protazil. He is going to continue his other medications and supplements:
1. SmartPak: senior flex and immune boost
2. Vitamin E
3. MicroLactin (amazing) to help with regrowth of his cells, inflammation, and pain.
As I’m doing research, and trying to come up with a plan of action, once again I am inundated with opinions…medication, exercise, holistic, massage, acupuncture, chiropractic, organic, shoeing, etc.
I know I need to continue therapy, or start a new therapy. But which one do I choose?
Do I go the holistic approach and work with an acupuncturist, chiropractor, massage therapist, and vitamins such as Vita Royals? Do I go organic? Or do I try Marquis? Another month of Protazil? Oraquin-10? Rebalance has been linked to a number of recent deaths in the past handful of months. If I go the organic or holistic approach do I run the risk of the disease progressing? If I go with the medication do I run the risk of yet another “treatment crisis”?
I contacted Vet4 and he suggested doing another round of the Protazil or Marquis. I decided on trying Marquis and waited for it to arrive.
Chance after a month on Protazil
Treatment Crisis (WARNING: DISTURBING)
Sure enough Chance experienced his very own treatment crisis about a week into treatment. The twisting of his back right hind was the worse it has ever been!
We gave him a dose of the Equinox (pain medication that is easier on his stomach) and the Ulcer Guard and wrapped his hind legs. He was on stall rest for about a week and was hand walked twice daily.
Below is Chance during his treatment crisis.

An All Natural Option?
While doing research on EPM, and ways to prevent a treatment crisis, I came across something called MicroLactin. Below are two of the many studies I found regarding the use of MicroLactin and its use for EPM.
STUDY 1: Journal of Equine Veterinary Science (Impact Factor: 0.89). 09/2005; 25(9):380-382. DOI: 10.1016/j.jevs.2005.08.004
STUDY 2: Sandhill Equine Center, Southern Pines, NC Journal of Equine Veterinary Science (Impact Factor: 0.89). 06/2009; 29(6):547-550. DOI: 10.1016/j.jevs.2009.05.004
Every study I read claimed MicroLactin to be a “miracle anti-inflammatory” that aided in cell regrowth. People were raving about this substance that is derived from cow’s milk. The studies dated back to the 80’s and not only suggested that MicroLactin truly was a natural cure all, but that it also had zero side effects or interactions.
I figured that I should give it a try. Again, I looked everywhere and nobody carried it. I looked online and saw that there was a brand called DuraLactin but that I would not be able to actually receive it for about a week. I began looking for supplements that contained the same ingredients as DuraLactin. Sure enough, I was able to find it!
The brand is called Vita-Flex Equinyl.
Vita Flex® Equinyl™ Combo is designed to help ease pain and inflammation associated with training and competition without causing gastrointestinal side effects. This supplement provides joint health support and increases flexibility. It shortens recovery time by reducing the emigration of neutrophils to the site of the inflammation. Contains glucosamine, which helps maintain synovial fluid that lubricates the joints for all day pain associated with daily exercise and activity. 5,000 mg glucosamine, 875 mg chondroitin. 7500 mg MSM. 3.75 lb (60-day supply).
How to we get there?
As I said previously, the idea of Chance collapsing and no one being there terrifies me. Vet4 is shipping me the Protazil and I am trying to find another vet to come and administer the DMSO before beginning treatment. DMSO typically helps the Protazil adhere better, thus making the treatment more effective.
EPM: Is DMSO the Cure for Treatment Issues?
By Stacey Oke, DVM, MSc Aug 3, 2009
New research on treating horses with equine protozoal myeloencephalitis (EPM) has found dissolving toltrazuril sulfone, commercially known as ponazuril, in dimethylsulfoxide (DMSO) instead of water prior to oral administration in horses increases the bioavailability by three times and achieves therapeutic levels in both the blood and cerebrospinal fluid.
Ponazuril and related triazine-based antiprotozoal agents used to treat horses with EPM are highly lipid (fat) soluble. As a result, these agents dissolve poorly in the gastrointestinal systemand are therefore poorly absorbed.
Poor drug absorption results in variable drug concentrations in the bloodstream, which translates into a variable therapeutic effect in the treated horse, explained Levent Dirikolu, DVM, PhD, from the Department of Veterinary Biosciences at the University of Illinois, and co-researchers from the University of Kentucky Gluck Equine Research Center and the United States Department of Agriculture (USDA) Animal and Natural resources Institute.
I finally found a vet who was able to come to the farm to meet Chance and administer other medications.
Vet6 felt that DMSO wasn’t necessary and that Chance would be fine. I called Vet4, explained the situation, and he advised beginning Chance on 1/2 a dose of Protazil for the first couple days in conjunction with a mild anti-inflammatory.
So, that is what we did. I had also read that Vit E (only in its all natural form) was helpful during treatment, along with Ulcer Guard to keep his stomach safe from the medications.
I called 5 different vets and no one has what I was looking for in stock. I finally found it in Chantilly!
Bello Article on EPM
Below is an attachment on the intensive approach to treating EPM.
Other EPM Therapies
The below research was found athttp://www.epmhorse.org/Treatment/Other_Therapy.htm
Veterinarians should discuss other drug therapies, in addition to the protozoa killing drugs, to address symptomatic problems that may occur during treatment. Limiting inflammation of the cerebrospinal column, stimulating the immune system, and anti-oxidants are three things that the owner should be prepared to handle during treatment. If the veterinarian does not discuss these, ask about them.
Inflammation
An active S. neurona infection in the central nervous system (CNS) will produce both temporary inflammation and permanent nerve damage. The inflammation can get worse when the protozoa start to die during treatment. This can happen as the treatment drug level builds in the CNS, and is known as a ‘treatment crisis’. Watch for symptoms to get worse 7 to 14 days after the start of treatment drugs.
Inflammation by itself can cause permanent nerve damage, so treating it is important. Veterinarians report that horses with higher neurologic deficiencies, and possibly higher levels of protozoa, tend to get treatment crises more often that horses with a Mayhew score of 1. Some veterinarians will place a horse on anti-inflammatory drugs immediately, to prevent additional damage to the CNS.
Banamine Many owners already have the non-steroidal anti-inflammatory drug (NSAID) Banamine at the barn. Even if your horse is a 1 on the Mayhew scale, you may wish to have Banamine on-hand to deal with any worsening of the symptoms. Banamine can cause gastro-intestinal side effects such as ulcers when given in high doses, or longer than five days. A January 2009 cost was $35 for 5 doses.
MicroLactin This supplement is gaining recognition as an overall, mild anti-inflammatory. This non-prescription supplement is a derivative of cows milk, and is known as Duralactin, or the ingredient ComfortX in Equinyl. MicroLactin does not have side effects, so it can be used over the entire course of treatment. It is possible to supplement with Banamine during a treatment crisis. March 2009 price was $50 per month.
Dexamethazone (Dex) This steroid suppresses the immune system, so it should not be used as an anti-inflammatory for EPM horses except in an extreme neurological case. Used longer than 5 days, it can cause Laminitis.
DMSO Dimethyl sulfoxide given intravenously, can be useful when the horse has extreme neurological symptoms. The veterinarian should administer this drug, it should only be used for short time periods, and it can interact with other drugs.
Immune System
In many regions of the U.S. more than 50% of the horses have been exposed to EPM. Researchers do not know why less than 2% of them get an active infection in the CNS. Studies on blood of EPM horses indicate a change in the immune system response and cells. Relapse rates for EPM are high, often with the same symptoms. Some researchers believe that the relapses are latent infections which were never completely killed, and the immune system does not recognize. Immune system stimulants have been suggested to help the horse fight the infection.
Levasimole This drug has been used as part of a wormer, and anti-inflammatory. It is known to increase immune response. It has not been clinically tested specifically for use with EPM, but is being used for it.
Transfer Factor This supplement has been around since the 1940’s for human use. The older studies on humans suggest it increases the cell-mediated immune response. It has not been clinically tested in horses. The supplement is suggested to increase the cell-mediated immune response (see research below). It WILL NOT kill the protozoa; it is only an immune booster. It is made from cow colostrum, eggs, and mushrooms. At least two companies produce this for equine use, and while the main ingredients are the same, there are differences. 4 Life Research and Nutrition Horizons USA offer this at March 2009 prices of $150 to $200 per month.
Vitamin E
Vitamin E has been shown to relieve inflammation, promote regeneration of nerve cells, and is an anti-oxidant protecting the CNS. This vitamin is suggested by many veterinarians for supplementation during and after drug treatment for EPM. It crosses the blood-brain barrier to work in the CNS. A deficiency in Vitamin E is thought to impair the blood-brain barrier. It is suggested at therapeutic rates from 5,000 to 10,000 total IU per day. Add the total Vitamin E content of all supplements and feed to reach the target rate. Research has shown that natural source vitamin E (D-alpha tocopherol) is absorbed by the body better than manufactured E (DL-alpha-tocopherol).
Recent Research
A 2006 study published in Veterinary Parasitology indicated: “Our results demonstrated that naturally infected horses had significantly (P < 0.05) higher percentages of CD4 T-lymphocytes and neutrophils (PMN) in separated peripheral blood leukocytes than clinically normal horses. The product MicroLactin has been shown to limit neutrophil activity thereby reducing the inflammation process in the CNS. The study goes on to say, “Leukocytes from naturally infected EPM horses had significantly lower proliferation responses, as measured by thymidine incorporation, to a non-antigen specific mitogen than did clinically normal horses (P < 0.05). Cell-mediated immunity is lowered in EPM positive horses.
An ongoing study by Dr. Bello, Journal of Equine Veterinary Science, vol. 28, issue 8 (2008), uses Marquis, MicroLactin, and transfer factor in a protocol. The initial study involved 28 horses, and 8 more have been studied. This study was presented at the AVMA conference in 2007, and was published in 2008. The full text article is available below with permission from Dr. Bello.
Continuing research by others indicates controlling inflammation is a large part of the treatment process, and immune system stimulation is critical to avoiding relapses.
January 2012
References:
Veterinary Parasitology 138 (2006) 200–210
J Appl Res Vet Med 2003;1:272-8.
J Eq Vet Sc, vol. 28, issue 8 (2008) 479-482
An Intensive Approach in the Treatment of Clinical Equine Protozoal Myeloencephalitis
Am J Vet Research, June 2008 Vitamin E
J Eq Vet Sc, vol. 25, issue 9 (2005) 380-382
TheHorse.com articles # 12025, 4829
“I will not get on that trailer!”
The treatment crisis terrified me. I decided to try to get Chance to the hospital.
Tried I did. For a total of 8 hours over the course of two days.
WE TRIED EVERYTHING!
Treats, grain, Quietex, walking, crossing lead ropes, talking, begging, pleading, more treats, another horse, a different loading angle, backing the trailer up to the barn doors, and 100000 other things. I even rubbed lavender oil on his face. After about 5 hours of trying calmly to coax him, I stopped.
The next day I decided to try it alone…just me and Chance….maybe the group of people was too scary? I noticed his ataxia was worse and remembered that stress can increase the symptoms. So, he and I walked and talked and I let him smell the trailer. Very low key. After 3 hours of walking and talking, he finally walked up the ramp…and decided, nope! That is when I knew that this wasn’t worth it.
He was scared and confused and that was okay. We will figure out what to do from here, like we have with every other obstacle over the last 6 months.
Yet Another Obstacle
Chance has been doing great since his Stem Cell treatment. He has not had a single flare up of Lymphangitis since he arrived in Sperryville. He no longer stocks up when he stays inside due to weather. He is gaining weight. AND he has not been on daily pain medication! He is finally happy, healthy, and pain free!
Until one day I noticed that he began twisting his back right leg inward at the walk. I figured that it was due to the long term injury to the DDFT and lack of muscle on that side. I asked Vet4 and he agreed. I called the farrier, who had previously worked on Chance when we arrived in Lynchburg many years prior, and he did a more supportive back shoe. The shoes seemed to help a bit- Chance’s twist was less extreme.
A few weeks later, I realized that I needed to find a local vet due to Vet4 being 2 hours away. I called and Vet5 came out. She watched Chance walk down a small hill and immediately said, “He is a wobbler! We need to test him for EPM.” I tried to justify Chance’s ataxia by suggesting that he was walking down a hill, after a long standing injury, and it was a bit muddy. And, to be perfectly honest, I was a bit peeved! My horse did NOT have EPM! Not after all he had already been through! He was healthy! He just needed some rehab to rebuild the muscle. I was thinking to myself, that EPM was the first condition that I had addressed with Vet1. The very same diagnosis he had shot down. There was no way….
Well, we tested him anyway. I convinced myself that the test would come back negative.
I began to do what I do best- hours of research. The journals and articles I read said, that while 50% of horses have come in contact with contaminated feed, only 1% actually develop symptoms! 1 PERCENT! The Protazia attack the CNS, eventually moving from the spinal cord to the brain. Symptoms can, and will, differ from horse to horse, but usually a horse with the parasite on the spinal cord shows lameness and ataxia on one side of the body (usually hind end). Where as horses whose brain has become infected, show anything from paralysis of the face, to personality changes, choking, difficulty chewing, etc.
A week or so later, I received a call that Chance did have EPM! I was heartbroken! And, honestly, I was angry! Angry at Vet1 for dismissing my initial thoughts about Chance having EPM! I was reassured that he was not in any pain, but in order to ensure his safety, we needed to get him on medication ASAP!
Again, hours of research…looking at the different medications (Protazil, Marquis, etc) and the outcomes and side effects.
I called the vet I trusted with my horse’s life, Vet4, and he walked me through what should be done.
Spoke to Vet4 ie EPM results:
He state there were two choices- Marque and Protazil & typically he sees an improvement with 85% of horses.
Plan:
Day 1: DMSO and Banamine
Day 2: Same
Day 3: Same
Day 4: Begin Protazil with DMSO and Banamine
After reading about my opinions, I was inundated with talk about what is referred to as, “the treatment crisis”. Some horses will begin the medication and, due to the kill off of the parasite, their body reacts with severe inflammation. Some horses will collapse and not be able to get back up, and others will have an increase in their initial EPM related symptoms. This scared me. I did not want Chance to fall and be laying there all alone for hours; I wanted him to be under 24/7 watch.
Vet4 said that If I wanted to trailer him to the hospital, I was looking at around $1500.00 for one month.
~$800.00 (1 month)
~$700 (1 month) board
Typically, the outcome of the medication, when EPM is caught early, is a decrease in 2 grades of Ataxia. Chance was deemed a 3 on the Ataxia Scale.






