The other day I noticed that Chance’s back fetlock a were slightly swollen and he was visably stiffer then normal. I also noticed a golf ball sized lump in the middle of the his chest. It wasn’t super sensitive and looked like a tick bite reaction, except there was no tick and a tiny barely noticeable scratch.
I put a Poltace wrap on his back right leg (which was the leg he had previously injured and received stem cell injections in) and gave him some pain medication. I also started him on Baytril and Ulcerguard as a precaution as previously advised by the vet.
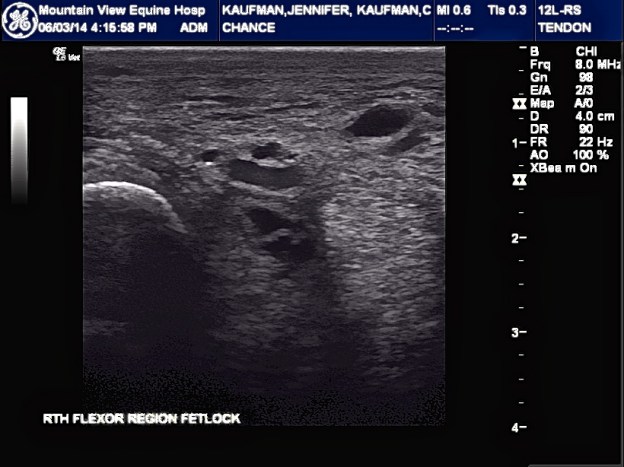
I made an appointment with our vet to come ultrasound his hind right leg and she was to come out in the next two days. I was incredibly anxious to say the least.
The vet arrived and explained that the lump on Chance’s chest was a hematoma from another horse biting him or from him hitting something. Nothing to worry about, it was just the pooling of fluids to lowest point.
I then trotted Chance back and forth as the vet watched. After an exam and the ultrasound, the vet explained that she felt that the swelling was due to Chance’s hip pain and the Pastern dermatitis that we have been treating and we’re finally coming off.
The ultrasound showed a tiny DDFT lesion (vet referred to as a defect that shouldn’t be causing any symptoms). The ultrasound also showed scar tissue that we need to get “stretched out” so that he can gain increased flexibility and work as a protection for Chance’s tendons and legiments. The ultrasound also showed some fluid build up as well. Chance’s Fetlock looks good as do his legiments.
The vet wants Chance to stay on Baytril and Ulcerguard until complete. She also has added a 5 day course of Benadryl and steroids to help with edema of back hind legs.
She also provided me with a shampoo that is milder to clean off scratches and apply swat after cleaning. The vet explained that she didn’t understand why people picked the scabs from the scratches because they’re super deep and pulling the scabs off does more harm than good.
The Vet commented on Chance’s weight gain and how great his skin looks gooded. She wants me to continue working on the scratches and continue doing physical therapy on hills to build up his hind end then get farrier out for back feet.
All and all I feel good about how Chance is doing and feeling. He is still full of energy, eats like he hasn’t eaten in a week, and his eyes and coat are bright. He is not on daily pain medication and is only given it when he is not feeling great. Aside from a few hiccups, Chance is loving life and being spoiled!