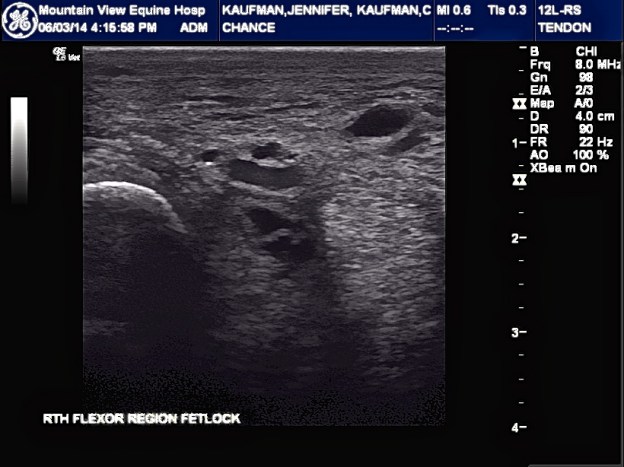
Text from Vet4 after ultra sound #3:
“I can see that he has a deep digital flexor tendon lesion and the medial side of the tendon sheath has improve but lateral side is about the same. The DDFT may the cause of all this in the first place and everything else is secondary. We will re ultrasound in 10 days or so just to confirm my findings. If they are correct, it would help to treat that area.”
Conversation with Vet4 :
So far, Chance has received; shock wave therapy, compression therapy and laser therapy.
Chance has a hole in his tendon. Vet4 believes that this is due to an infection/bowed tendon and severe lameness. The ultrasound, done yesterday, shows no change in size of the tendon hole after the previous two rounds of injections.
“Lymphangitis is a symptom rather than a cause and the cause was never treated.” Vet1 continued to treat it like a disorder rather than a symptom!
The swelling and infection have dissipated, as has the severity of the lameness. Though still lame, he is running around in the pasture.
Pain meds were started again due to increased discomfort and soreness.
Vet4 suggests doing one of the following:
1. Stem cell- which can take about two days if sample drawn has enough stem cells. If not, it could take about 4-6 wks to culture. Once injected he can move home. He is to be hand walked for a few days and then can go out as normal. Vet4 will come out in about a month to do another ultrasound and, depending on the size of the hole, may need to do further injections.
2. Surgery to clean out but NOT repair the tendon. This was not discussed in detail.
Payment plans may be an option. I emailed the office for payment options.
Time to make another decision!








 The month passed by slowly….I kept hitting a brick wall over and over again…with each diagnostic test we ran.
The month passed by slowly….I kept hitting a brick wall over and over again…with each diagnostic test we ran.




