Such a perfect day to lay on the grass and read!
Category Archives: Thoroughbred

Eyes Wide Shut
I had the opportunity to work with a “horse communicator” today. She was recommended to me by an equine vet who, after reading my blog, felt that I would be open to the idea, and introduced me to her via email. According to the vet, she often works with this particular equine communicator due to her ability to point out exactly where the horse’s issues are, allowing the vet to adjust/manipulate/treat the main issue.
I chatted with her at length a few days ago as she explained the process and we scheduled an appointment.
Today I gave her a call, as she explained, connecting remotely allows for the horse to be in his natural setting without the influence of an unknown person. That way the horse could be relaxed and the owner can observe, ask questions, and engage. So, that is what I did. She went onto explain that sometimes the horse needs energy work in order to open up to the process and that the horse must trust the process, her, and obviously, the owner.
I was asked to have questions ready to ask my horse, along with something I would like to tell him at the end of the session. (If you have been following this blog then you will know I had some difficulty narrowing down a couple of questions- I have a lot! 😉 ) She began connecting with Chance.
I will not be able to convey all the details of what was said, Chance’s reactions, or even mine…It is almost a blur… I wish I could.
I was asked to feel around Chance’s right forehead/eye area for a lump or bump. I did as I was asked and didn’t feel anything abnormal…but remembered he had a gash that was healing right above his right eye. She informed me that he had a “headache”. She continued to move over him and explained that his “energy” was “blocked” on his right side. This makes sense…Chance has a “swagger” at the walk- he pokes his butt to the side and has a twist on the back right leg (Chance’s swagger has gone up and down- it was worse when he had the tendon issues, resolved after stem cell injections, came back when he got EPM, went away ish, and came back with his Lyme). While she was working on his energy, I massaged Chance’s back, neck, hip, and shoulders. She went on to explain that Chance had some right shoulder pain. Thankfully, Chance allowed her to work on his jaw (he pretty much has TMJ), his head, his back, etc. The energy was “pouring out” even on the hind end which, if I recall correctly, is commonly seen on horses with head injuries.
This is where my one question came in…I wanted to know what happened to Chance when he came to my college. I didn’t give many details…I didn’t know many details but I always wondered what may have happened on Chance’s trip down to my college.
I had gone off to college in January and decided to have someone trailer Chance down (about 3 and a 1/2 hours) once I got settled and found a barn, etc. Two months later Chance was arrived at her new barn. Despite the cool March weather, he was covered in sweat and was visibly scared. I didn’t inquire too much since he was in one piece and I chalked up the sweating and fear to exactly that- fear and anxiety. However, as the months progressed, Chance began bucking and rearing while under saddle….this was really strange..When he had left home we were doing dressage and jumping and he was sound and calm. Once again, I chalked it up to being in a new place- a barn that hosted Friday night Bullbucking no less. I decided to switch to a different farm, one preferably without bulls, even though the show was awesome to go and see, and work with a trainer. Still the behaviors persisted and the episodes of lameness increased. The vet finally diagnosed Chance with arthritic changes in his back and suggested I no longer jump him. I decided that summer instead of bringing Chance home and have him endure another long trailer ride, to board him at my new vet’s farm. Chance had the summer to recuperate while under the care of an equine vet.
Anyways, after that summer, I decided to retire Chance for good. I would occasionally get home him to walk around, I still can and do today. But, that was the beginning of a chronic condition that was never given a diagnosis. Instead, Chance’s symptoms were treated as they came.
Back to my session with my very own horse whisperer..
Chance “showed” her what happened on his trip to college- a trailer wheel falling off the side of the road. His head hitting one side of the trailer and slamming the other side. The pain. The concussion. His neck and back becoming misaligned. His jaw coming out of position. His body compensating. He showed the decline of his once functioning body- starting with the hit on his head, to his jaw, and his neck. Down his neck and through his back towards his hips and down his legs. The wear and tear of his body. Chance stated that he is still angry with the person driving the trailer; he wasn’t ready to forgive. I have forgiven them. I have no doubt it was a mistake and that there was no ill intent. But, I am not the one feeling the pain that he is. I am not the one who went from a racehorse to a jumper to practicing dressage to retirement long before I should have. And like the “horse whisperer” said, she will “hold the forgiveness for him until he is ready.” I will do the same.
She spoke of his time on the racetrack. Chance was happy to hear that he was being remembered for who he once was, and will always be to me- a strong, beautiful and crazy talented 17.1 hand red-headed thoroughbred and not a “weak old man” as he put it. When asked what his name was during his time on the track, he said, “Hot Stuff”, which could be a nickname and not his actual race name.
At one point during Chance’s session he fell asleep; standing in an odd way- hind legs spread out. Suddenly, his body gave out and he caught himself from falling. This entire time his eyes were still closed! They remained closed for another minute after this. His body reacting to something, perhaps a shift in his energies, and all the while he was a a state of peace; trusting that nothing bad would happen to him.
The session lasted an hour and a half. Honestly, we could have continued because of all the “blockages” but decided to stop for the day and pick up again another day. I was told that the effects of the energy work or Reiki, would continued throughout the week and that he would be emotionally vulnerable. As the session wrapped up Chance apparently said that he was the lucky one because I found him all those years ago.
Energy Work and Reiki Resources
Reiki for Horses: Workshops, Training, Courses, and Resources
Reiki Related Research and Resources for Two and Four Legged Friends
Amorosa Equestrian Center in Ohio
Reiki Forum on Horse and Hound
Reiki Handout: Full history, explanation, and how to pictures
Equine Communication
Horse Forum: Horse Communicators
Head Trauma and Headaches in Horses
Symptoms of Equine Concussions
Trauma, Concussions or Other Brain injuries in Horses
How to Handle Horse Head Injuries
Helping Horses with Traumatic Brain Injuries

EPM Tilter. What Do The Numbers Mean?
During my horse’s recent Lymphingitis flare-up, the vet advised that we run labs to test for Lyme and EPM due to his presenting symptoms (hind weakness, twisting his back leg at the walk/walking sideways I refer to it as- “Chance’s swagger”). As I noted previously, Chance’s Lyme test revealed that he was at the beginning stages of an acute infection…yay for the labs at Cornell University for their amazing ability to give you more than a positive or negative!
A little history before getting to the EPM Tilter results.
About 2ish years ago, Chance was diagnosed with EPM (and one of the reasons opossums and I are not friends since they host the disease as do a few other culprits). Chance immediately began EPM treatment- he received Protazil in his feed for one month. After hours of research I chose Protazil, although extremely expensive (if you order from http://www.drfosterandsmith.com they sometimes have promotions where you receive store credit for every $100.00 you spend…they did when I ordered and I got a “free” dog bed that my dogs adore), due to the decreased likelihood of Chance experiencing a “Treatment Crisis” (worsening of symptoms) and the ease of administration (other brands require the drug being administered 1 hour before eating or an hour after and so on). Typically, EPM treatment is done for 30 days and, depending on the residual symptoms, some may require subsequent treatments. While Chance’s symptoms improved, I wanted to ensure that we annihilated the disease and did another round of treatment but this time with Marquis. At the end of two months, Chance’s ataxia was gone!
Fast forward to September 2016…Chance, just having a Lymphingitis flare-up, has been tested for Lyme and EPM. Lyme came back positive. And….so did the EPM test..well, kind of. Wonderful. (See why I loathe opossums?)
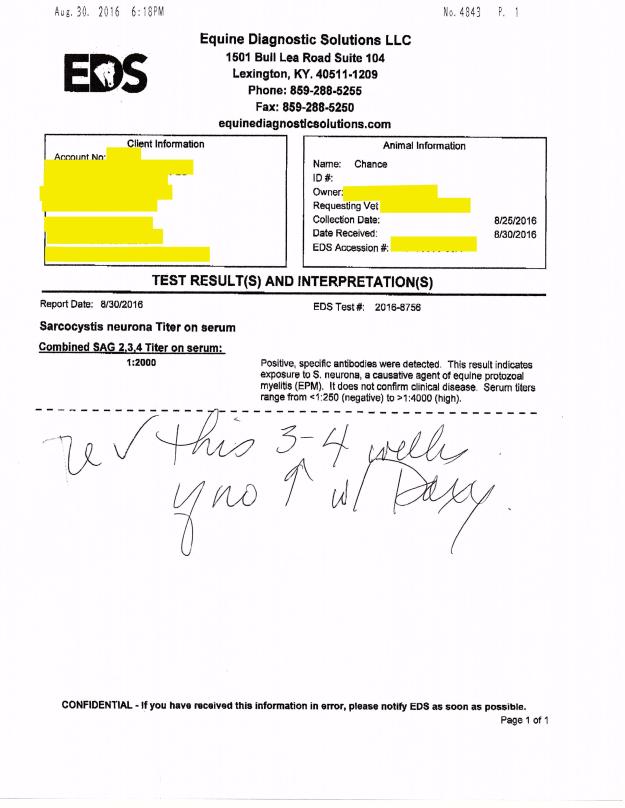
Chance’s EPM test #2 on 8/30/16 (the 1st one was 2ish years ago) showed the following:
“Combined SAG 2,3,4 Tilter on serum= 1:2000”
So, what does this mean?
The test revealed that Chance had “positive, specific antibodies” detected in the blood work. This means that he had EXPOSURE to S. Neurona, a causative agent of EPM. Serum tilters range from <1:250 (negative) to >1:4000 (high positive). S. Neurona (SarcoFluor) is one of two protozoa found in EPM infected horses, the other protazoa is N. Hughesil (NeoFluor). S. Neurona is most frequently seen, whereas N. Hughesil is not as common.
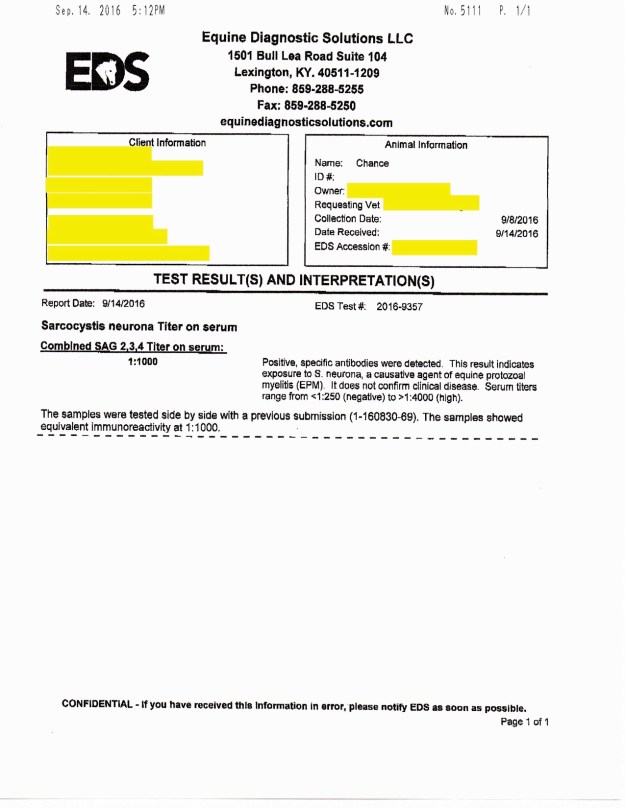
The vet ran another EPM test to confirm the findings in the 8/30/16 test. The results showed that Chance had “Combined SAG 2,3,4 Tilter on serum= 1:1000. Again, Chance showed EPM protozoa in the positive-ish range.
I initially had not seen the results but was told by the vet that he was EPM negative. So when I asked for the test results to be emailed to me and saw the numbers I sort of freaked out…I emailed the vet to ask for clarification. She explained,
“The EPM test shows that he was exposed to the organism in the first test we did which is why we did a follow-up test. Since his exposure level dropped from 1:2000 to 1:1000 this shows that he does not have the disease. There is no good one time test for EPM once they are exposed which is why we had to do the repeat to compare the two.”
While this explanation offered me comfort, I was confused…why does he have any protozoa in his blood if he doesn’t have EPM?
I spoke to another vet and she explained it in a bit more detail…I am hoping I am summarizing what she said correctly..
When a horse tests positive for EPM they either have an active disease or they may not. However, when the test does from 1:2000 down to 1:1000 this typically means that the horse’s immune system is working correctly to fight the disease off- active or not. EPM testing typically provides you with a % of the chance your horse has an active EPM infection, or at least if you send it to Cornell University. For instance, lets say a horse gets the results back and it shows that they are “positive” or have been exposed to S. Neurona (one of the two EPM protozoa)…their results are 1:647. This means that, after doing a bunch of adding and multiplying that this vet kindly did for me, the horse has a 60-70% chance of having ACTIVE EPM. Meaning, he most likely would be symptomatic (ie: behavioral changes, ataxia, weight loss, difficulty eating, changes in soundness, and a bunch of other neurological symptoms).
My hunch is that Chance’s immune system was boosted because I started him on Transfer Factor (amazing stuff… more information can be found in some of my older posts) again as soon as his results came back positive for Lyme.
Here are the 3 EPM tilters that were run on Chance (oldest to most recent) along with his Lyme test results:


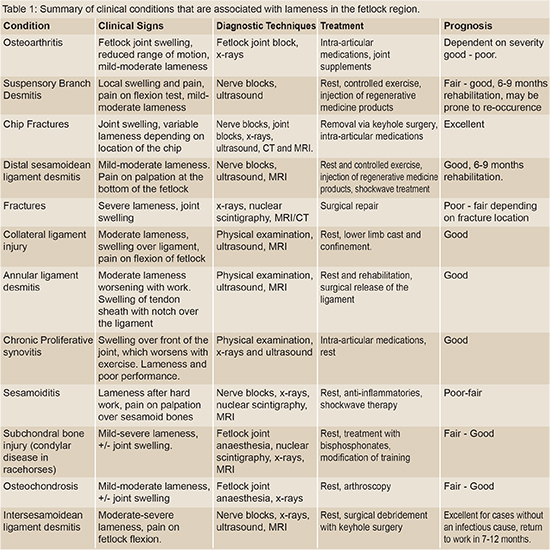
I have a limp!
Resources on how to diagnose, treat, prevent, and handle lameness in horses
Your Horse Has a Swollen Leg – Why and What To Do | EquiMed – Horse Health Matters
Fetlock Lameness – It’s importance… | The Horse Magazine – Australia’s Leading Equestrian Magazine
Causes of Equine Lameness | EquiMed – Horse Health Matters
Common Causes of Lameness in the Fetlock

Flower Horses

Equine Podiatry
Medical History
- DDFT Lesion on right hind
- Cervical Spine Arthritis
- Hip discomfort due to past fall
Past Treatments Tried
- Stem Cell Injections: Healed the DDFT lesion in right hind until recently the lesion began to reappear
- Ozone Therapy: Assists in the healing of tissues
- Shock Wave Therapy: Assists in the healing of tissue
- Chriopractic adjustments
- Acupuncture
- Supplements
Initial Consultation
Chance showed decreased movement in his right hip and a audible cracking noise at the suspensory joint. He has edema of both hind fetlocks, Pastern, and Pastern Dermatitis. Chance was unshawed on both hinds due to his inability to stand for long periods of time and his decreased mobility. However, his front adorned clips.
Due to the length of Chance’s front toes and the height of his heels he was unable to evenly distribute his weight (60/40) to his front and hind ends. This would most likely cause increased tension on the DDFT tendons and corresponding ligaments resulting in an increased likelihood of tendon and ligament related injuries. The uneven distribution of weight could also inhibit the horse’s range of motion through his hips resulting in his body compensating for this injury and causing ataxia (balance issues), pain, arthritic changes, and cervical spine misalignment.
By shortening the toe of both front feet, the heel will rise allowing a more even distribution of his weight.
Front


Final Product: Front
Trimmed feet to corrected to the following specifications:
Foot Beginning Angle & Toe Corrected Angles & Toe Total P.C.
L/F 47 Degrees at 3 7/8 inches 53 Degrees at 3 inches 6 Degrees
R/F 45 Degrees at 3 3/4 inches 54 Degrees at 3 inches 9 Degrees
Hind

Final Product: Hind

| Return visit to trim and shoe Chance’s hind feet with #2 OBRHB Wedge shoes.Trimmed hind feet and corrected to the following specifications:
Foot Beginning Angle & Toe Corrected Angles & Toe Total P.C. L/H 48 Degrees at 3 7/8 inches 54 Degrees at 3 1/4 inches 6 Degrees R/H 46 Degrees at 4 1/4 inches 55 Degrees at 3 1/4 inches 9 Degrees Note: Chance needed to be sedated by veterinarian to complete the trim and shoe his hind feet due to preexisting hip and DDFT issues. |

Ozone Therapy
OZONE THERAPY – HISTORY, PHYSIOLOGY, INDICATIONS, RESULTS
Judith M. Shoemaker, DVM 305 Nottingham Road Nottingham, PA 19362
717-529-0526 Fax 717-529-0776
http://www.judithshoemaker.com
Ozone therapy has been utilized and heavily studied for more than a century. Its effects are proven, consistent, safe and without side effects. Why is it not more universal in its use? Many of you have come with some trepidation about infusing a gas into a vessel because you are concerned about emboli, or have some dreadful fear about ozone’s toxicity since we frequently hear about the unhealthy ozone levels in the atmosphere. These fears do not apply to properly administered medical ozone, and the potential benefits of ozone therapy are profound and without associated detrimental effects.
Oxygen, in its several forms, cycles through the atmosphere and life processes just as water does. Ozone is produced in the upper atmosphere when UV light strikes the oxygen rising from plants, plankton, and algae in our forests and seas. It then falls back through the atmosphere, as it is heavier than air, combining with pollutants and water, cleaning the air and forming peroxides that benefit plants. Ultraviolet light breaking down pollutants and nitrous oxides also can produce ozone at the ground level, which is the eye and lung irritant in smog.
Medical ozone, used to disinfect and treat disease, has been around for over 150 years. Used to treat infections, wounds, and multiple diseases, ozone’s effectiveness has been well documented. Ozone has been used to disinfect drinking water since before the turn of the last century. A text on medical ozone therapy was published by Dr. Charles J. Kenworth in 1885! The best technology for producing ozone gas was designed and built by Nikola Tesla in the 1920’s. Heads of leading medical institutions in the U.S. contributed to a 1929 book “Ozone and Its Therapeutic Actions” describing the treatment of 114 diseases using ozone.
In 1933, the AMA began its systematic suppression of all modalities of treatment that did not complement its liaison with the emerging pharmacologic and diagnostic industries. Ozone therapy, along with many other useful therapies, were methodically eliminated from the educational process and exposure to the public in the U.S.
Less suppression has occurred in Europe and other countries, especially in Russia. Today in Germany, and other countries, ozone therapy is commonplace. Over 7000 doctors in Germany use it daily. In fact, in Germany, ozone generators are in ambulances for treatment of stroke victims. The incidence of permanent paralysis in these patients is much less than that in similar patients where ozone is not used.
Ozone generators are relatively simple and inexpensive. The equipment used to handle ozone is readily available but needs to be relatively non-reactive. Glass, Teflon, Kynar, silicon, and gold are completely non-reactive. Equipment made of other substances can contaminate the ozone or just deteriorate rapidly using up the ozone and becoming nonfunctional.
Generators use several technologies to produce ozone
- UV lamp – makes small amounts of ozone and is unreliable in making accurate concentrations. They burn out easily.
- Corona discharge – dual dielectric sealed systems produce ozone but also lots of heat which is both destructive to ozone and to the machine.
- Cold plasma generators – which produce ozone using low level current passed in 2 tubes of a noble gas between which an electrostatic plasma field forms that ionizes the oxygen.Ozone concentration is measured in u/ml or gms/L of oxygen, 5% or 70 u/ml is usually the maximum concentration used in clinical medical applications. High concentrations will damage red cells and inhibit growth of healthy cells.Dosage and frequency protocols vary widely. Initial high dose treatments may “jumpstart” the immune system followed by lower doses. Those who are fearful have been “starting slow and going low” with dosage and still have good results. Concentration must be carefully controlled with accurate flow rates, requiring pediatric regulators for the needed slow flow rates to produce high concentrations. Therefore, home made machines and lesser quality nonmedical devices are not appropriate.
Ozone poteniates free radical scavenging substances and systems in the body, inducing the production of superoxide dismutase, catalase, and glutathione peroxidase. If ozone administration causes any respiratory irritation from out-gassing through the lungs, a bolus dose of 1 to 5 grams of vitamin C can be given and will eliminate any coughing instantly.
Oxygen/ozone mixtures cannot cause emboli when injected at reasonable rates as they dissolve and diffuse very quickly in body fluids, unlike air (predominantly nitrogen) which is what forms emboli and causes the bends or decompression disease.
The physiologic actions of ozone are many, the simplest of which is to provide sufficient oxygen to allow complete oxidation of sugars and other fuels to produce sufficient and efficient energy and to “burn clean” to CO2, water, and inert end products. If not enough oxygen is available, then incomplete oxidation occurs, producing carbon monoxide, lactic acid, and partially oxidized toxins that inhibit further oxygen metabolism and “clog the system”, tying up hemoglobin, water, and the mechanisms for function and elimination.
Administration can be through any route with modifications:
- Direct IV infusion – Ozone slowly administered into a major vessel.
- Major auto-hemotherapy – Anticoagulated blood is mixed with ozone and is infused into a vessel.
- Rectal/vaginal insufflation – Humidified ozone is administered by catheter.
- Minor autohemotherapy – Blood mixed with ozone is injected intramuscularly.
- Limb or body bagging – Body or parts are bathed in humidified ozone.
- Ozonated water – Dissolves easily in water to be used topically or consumed.
- Ozone in Saline or LRS – Can be used topically or given IV or SQ.
- Intra-articular administration – For joint healing and prolotherapy.
- Prolo/Sclerotherapy – Very good, less painful than other agents.
- Acupuncture – With ozone, more effective than B12.
- Ozonated olive oil – Ozone is bubbled through oil until the oil is thickened. This will produce ozonides that are not irritating and thus is applied topically even to eyes.
- Inhalation – Ozone that has been bubbled through olive oil and humidified will not irritate respiratory epithelium.
- Subconjunctival injection – For ulcers and keratitis sicca.
- Gingival and tooth apex injection – Can eliminate infection.
- Urinary bladder insufflation – For chronic inflammation.
- Disc protrusions – Prolotherapy, which can be injected at interspinous space and around facets, stabilize joints and accelerate healing.
- Auricular – Can be direct, humidified, or bagged with a homemade device made from IV bags and tubing (á la Margo Roman).As an anticancer, antiviral, antibacterial, and ant fungal agent, ozone is unsurpassed, especially since there are no appreciable side effects.Oxygen deficit is key to the development and progression of all disease processes. Dr. Otto Warburg’s work, confirmed by others, shows that this deficit and subsequent toxin buildup is the fundamental cause of all degenerative disease, especially cancers.
Antioxidants help the body to protect itself from excessive oxidative damage caused by multiple free radicals, many of which are inactivated by ozone. The support of free radical scavenging systems is important but only oxygen can improve the deficit that makes cells vulnerable to oxidative damage in the first place. Long-term ozone therapy can be augmented by supplementation with antioxidants, but normally they should not be administered within 4 to 12 hours of ozone therapies.
Ozone produces the same effects as exercise, which produces significantly more free radical oxygen than can be administered in any ozone treatment. Ozone equals ”exercise in a syringe” without doing joint damage.
Ozone potentiates more complete oxidation, helps to maintain more normal body temperature and increases the effects of most hormones, vitamins, herbs, homeopathics, and drugs. Concurrent ozone administration reduces the amount of chemotherapeutic drugs needed to achieve effect by 1⁄4 to 3⁄4. It complements chelation therapies and frequently improves the affect and sense of well being in patients.
Continued therapy will allow Herring’s Law to manifest “Healing from inside to outside, top to bottom, front to rear, and in reverse chronological order of the insults to the body.” Healing crises, however, may occur. Ozone therapy facilitates the rapid resolution of these crises.
2005 Judith M. Shoemaker, DVM

If You Experience Worsening Depression…
Chance began another round of Excede to get his scratches under control- it is a never ending battle. A while back, I had a skin scrape of Chance’s scratches due to their chronic nature. The scrape results showed a number of bacteria, all commonly seen with this type of infection, that were resistant to most antibiotics. Thus why we decided to try Excede.
Administering Excede is pretty straight forward- 1 shot IM every 4 days for about a month. Easy enough….or so I thought. The first shot was administered by the vet when I was not present. The second shot the vet also administered while I was there. Thirty minutes after the shot was given to Chance I noticed he seemed off but not in his “normal” post-acupuncture relaxed state. He suddenly became lethargic, he wouldn’t eat his dinner, and the gut noises became almost nonexistent. I commented to the vet my concerns and she came over and reexamined him. Sure enough something was wrong. She proceeded to administer 10cc of Banamine (just in case it was colic) and told me to walk him around outside for about 20-30 minutes. Then see if he would eat 2 cups of feed only. We walked and Chance began to act like his normal happy go lucky self. Once inside he started to eat!
Part of me felt that his reaction was a fluke. However, the third dose proved me wrong. Four days later, Chance received his shot and went outside to enjoy the first beautiful, warm day. I sat in the field watching him. He was sluggish, lethargic, stiff..he looked 10 years older and barely moved from one spot under a tree. He wasn’t eating grass nor did he run around and play- he didn’t even run up to me like he normally would. I decided to bring him inside and give him a warm bath since it was in the high 70’s. He was non responsive to his bath- no playing with the hose or even accepting peppermints. I placed a cooler on him to ensure he stayed warm until he was out in the sunshine. I figured after a bath he would perk up- again, I was wrong. At dinner time I went to bring him in and typically I will open up the gait and he will canter into his stall- he slowly walked instead. He wouldn’t eat his feed (he normally whinnies and makes a fuss until he gets his feed and devours it) or his hay…I stayed and watched him for a while and he just slept. I spoke to John, the guy who helps me with Chance and Lucky, and he confirmed that Chance hadn’t been finishing his feed and wasn’t running when he brought him in for dinner.
My concerns grew and I decided to do some research on Excede. That strange thing is I usually do extensive research before changing or administering anything with my animals. But, for some reason I did not do so this time and I wish I had.
According to a number of reputable websites, Excede can cause significant and dangerous side-effects such as; diarrhea, severe acid reflux, blood coming from mouth, loss of appetite, lethargy, muscle and gait stiffness, and more.
The most troubling of everything that I read wasn’t what was posted on the Pfizer (the manufacturer) website but from the countless statements given by horse owners and the studies done by outside companies.
According to drugs.com, “in the PK study, several horses developed clinical signs consistent with foot pain (stiff in the front limbs when turned in tight circles, and increased pulses and heat to the front feet). One horse in the NAXCEL group and one horse in the 6.0 mg/lb (2X) EXCEDE group were euthanized due to laminitis. Clinical signs of foot pain (stiff front limbs and increased heat and pulses in feet) affected more horses, for a longer period of time, in all EXCEDE-treated groups as compared to the NAXCEL-treated group. The study housing (multi-horse pens on concrete slabs) and diet (free choice alfalfa/grass mix and once a day pellets) may have contributed to the development of foot pain. The prevalence and severity of injection site reactions in EXCEDE-treated horses may also have contributed to the development of a stiff gait. A causal relationship between ceftiofur and foot pain could not be definitively determined.”
The research has revealed that Excede should be used with caution and the horse receiving the medication must be monitored. Make sure to weigh the benefits and risks before starting Excede. This drug can be lifesaving for many horses but for others, it can be life-threatening.
Excede Resources
Straight from the Horse’s Mouth: Antibiotics, Antifungals, Antivirals
Equine Product Catalog: In depth understanding of equine medications
FINALNewMexicoEIBPetitionExhibits2908-1407_pdf

Who Are You?
I have been trying for years to read Chance’s tattoo. Unfortunately, the tattoo was faded even back in 2000 and has become that much more over the years.
I have tried everything I can think of to figure out his tattoo or gain any information that I can about his racing name- video, photos, lots of light, a flashlight, a blue light, red light, asking vets and dentists, emailing his previous owner, the farm where I purchased him, my past trainers, rummaging through my old files…nada!
I have searched for hours on Jockey Club using his markings (white marks on his face and legs, different letter and number combinations based on his age, and different variations of what I thought was his “racing name”). I have even done a guided search that came back with nothing.
Chance’s racing records do not matter in the grand scheme of things…it is more curiosity then anything else. Plus, I think it would be pretty cool to find out more about my guy.
So far all I have is;
GENERAL IDENTIFICATION:
Horse Name:
Tattoo Number: T_____
Foaling Year: 1990
Color: Chestnut
Sex: Gelding
OTHER IDENTIFICATION:
Head: Patch of white hairs mid to top of eye level
Head Cowlick(s): Median cowlick at top of eye level.
Neck Cowlicks(s): Middle of front of neck
Left Fore Leg: cornet white left side of heel white
Left Hind Leg: none
Right Hind Leg: some white on cornet band
Right Fore Leg: none
Body: top of head off center/right behind right ear small white patch
Other: left foreleg inside firing markings
Resources
“You Are What You Eat…”
Chance has gained almost 1000 lbs in over a year and he could still use a few pounds. He lost wait quickly when he became sick.
Chance also has some factors that put him at a higher rate of weight loss and an increased difficulty maintaining and gaining weight.
- he is a senior horse
- a thoroughbred
- a cribber
- had an injury which caused him to not run around as much thus losing muscle mass
I slowly upped over the last year, with advisement from a nutritional specialist (her information is at the end of the post along with the name of her book which I found extremely helpful) and my vet, his feed from 3qt twice a day to 11qt twice a day.

Chance’s current regiment includes:
AM:
- Two 4qt scoops of Nutrina Safe Choice Senior feed
- One 3qt scoop of Timothy and Alfalfa pelleted mix
- I add his supplements
- 2 scoops of Body Sore (All natural supplement)
- 2 scoops of Cervical Formula (All natural supplement)
- I mix it all together with warm water so that it is sloppy (this makes it easier for him to eat at his age and lessens the chance of choking. Plus, it helps keep him hydrated especially in the winter when he is less inclined to drink as much water).
PM:
- Two 4qt scoops of Nutrina Safe Choice Senior feed
- One 3qt scoop of Timothy and Alfalfa pelleted mix
- I add his supplements
- 1 Smartpak (Senior Formula, Immune Booster, and Vitamin C)
- 2 scoops of DuraLactin (All natural anti-inflammatory and pain reducer derived from cow’s milk also called MicroLactin)
- 2 scoops of Body Sore (All natural supplement)
- 2 scoops of Cervical Formula (All natural supplement)
- I add about 5 flakes of hay (Alfalfa mix)
- Two 3qt scoops of hay stretcher in a separate feed bucket for snacking through the night

(Chance’s feed before adding water)
I also make sure that he eats his feed from a bucket on the ground. According to my vet it is the best way for a horse to eat.
Here are Some Nutrition Resources



Pain in the Neck
My old guy has always had issues with his cervical spine/neck. Throughout the years he has developed arthritis which has caused symptoms which mirror EPM such as; ataxia, difficulty bending, hind end weakness, difficulty going up hills, lethargy, difficulty balancing when foot is lifted, muscle atrophy, sore back…you get the picture.
When his symptoms first came on I had the vet test for EPM. The test was positive. I did my research and found out that about 50% of horses will test positive for EPM but only 1% show actual impairment from the virus. I went ahead and completed two rounds of EPM medication therapy and still his symptoms continued. So, I sought out another vet who practiced eastern and western medicine.
After some chiropractic adjustments and acupuncture she felt that his issues were actually due to the cervical spine and not EPM. The vet also showed me how, when looking at Chance straight on, one of his eyes was lower then the other- a classic sign of cervical and jaw issues. We continued with the chiropractic and acupuncture therapy and have continued for over a year and the change has been remarkable. Along with these therapies, we upped his feed, added supplements, began stretches and different exercises, and had him walking and running up and down hills whenever he was outside. The dentist has also been of great help by floating Chance’s teeth every few months instead of once a year. This helps with the alignment of his teeth because he tends to ware one side of his teeth down more then the other; ultimately straining his jaw and neck.
He has rebuilt the muscle on his hind end, put on around 100 lbs, and is able to do stretches while someone is holding his foot up. He runs when he is outside and is no longer on pain medications (except on the rare occasion).
Here is some useful information on a horse’s back and cervical spine.
Diagnosing A Horse’s Neck Problems
Main Causes of Ataxia in Horses

How To Read Equine (Horse and donkey) Blood Work?
I had the vet run some blood work on Luck and Chance as a precaution, because of the “Panic Grass” in Virginia has been causing liver failure in horses, and because I like to do a full work up every 6-12 months.
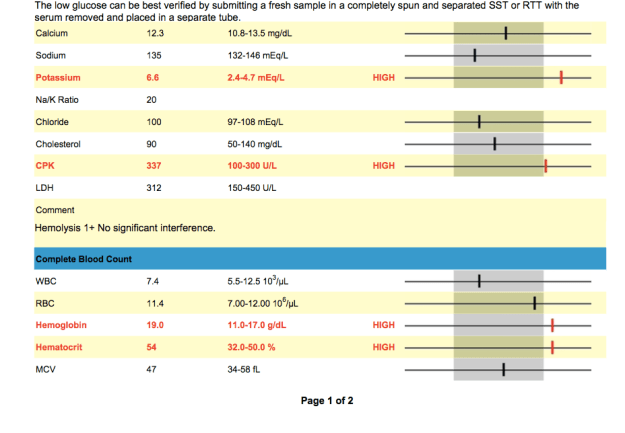
Chance’s Blood Work



INTERPRETATION OF RESULTS
Elevated Potassium (6.6 mEq/L):
Low Sodium:
“Low levels commonly indicate loss through excessive sweating, or through kidney or intestinal disease. Low levels may also be found in young foals with bladder damage. Increased sodium levels are usually a sign of dehydration” (http://www.minstervets.co.uk).
Low Platelets:
This was the most worrisome in regards to the potential immediate issues that could ensue because of the low platelet count.
Low Glucose:
“Glucose is the source of the body’s energy. It is measured in suspected cases of equine metabolic syndrome and sometimes in cases of equine Cushing’s disease. Blood glucose may also be measured as part of a glucose tolerance test, assessing small intestinal function” (http://www.minstervets.co.uk).
Levels 2-3x the highest number in range are considered significant according to vetstream.com. Levels are easily increased due to poor handling techniques as well as lab error.
According to Dr. Christine Woodford and Carla Baumgartner on vipsvet.com, “Elevations of CPK and SGOT are indictors of muscle inflammation–tying-up or rhabdomyolysis. The term “rhabdo” means muscle and “myolysis” means rupture of muscle cells. The CPK and SGOT are very sensitive indicators of skeletal muscle damage, and they rise in concentration proportionally with the amount of damage. A bit of timing is required in order to obtain the most sensitive results; CPK rises (due to its leakage from muscle cells into the blood system) approximately six to eight hours after the onset of muscle inflammation, and SGOT rises after approximately 12-14 hours. The absolute peak of CPK concentration and the time it takes to return to normal are important indicators of the severity of muscle damage and the response to therapy.”
Elevated MCV: Is the average volume of red blood cells.
- Macrocytosis.
- Indicates immature RBC in circulation (suggests regenerative anemia).
- Very rare in the horse, but may observe increasing MCV within normal range as horses increase erythropoiesis.
According to Vetstream.com, “Macrocytosis (increased MCV) resulting from release of immature RBC from the bone marrow during regeneration is very rare in the horse therefore the MCV is less useful in the horse than in other species.”
Elevated MCH: Is the average amount of hemoglobin in an individual red blood cell.
- Hemolysis, if intravascular in nature .
- Errors can occur during processing
Low RBC:
Luck’s blood work

Elevated Potassium: Potassium can become elevated for a number of reasons.
According to Vetstream.com,
- 98% of potassium is intracellular.
- Changes in serum or plasma potassium levels reflect fluid balance, rate of renal excretion and changes in balance between intra- and extracellular fluid.
- Hypokalemia increases membrane potential, resulting in hyperpolarization with weakness or paralysis.
- Hyperkalemia decreases membrane potential with resulting hyperexcitability.
- Results can be false due to processing time (ie: if the lab waited too long to process blood sample)
- Immediately after high intensity exercise.
- In association with clinical signs in horses with hyperkalemic periodic paraysis (HYPP) .
- Bladder rupture (neonate) .
- Hypoadrenocorticism [Pituitary: adenoma] (rare).
- Metabolic acidosis.
- Acute renal failure .
- Extensive tissue damage (especially muscle).
- IV potassium salts, eg potassium benzyl penicillin, potassium chloride .
- Phacochromocytoma (rare in the horse).
Hypokalemia - Chronic diarrhea.
- Diuretic therapy, especially potassium-losing diuretics.
- Excess bicarbonate/lactate therapy.
- Chronic liver disease .
- Acute renal failure (polyuric phase) .
- Recovery from severe trauma.
- Metabolic/respiratory alkalosis.
- Prolonged anorexia.
- Recovery period after high intensity exercise (30-60 min after).
- Parenteral feeding.
In combination with clinical signs and results of other tests results could signify the following;
- Muscle injury .
- Acute renal failure .
- Diarrhea.
- Tissue injury.
- Acid-base balance.
Elevated GGTP:
* Donkeys tend to have 3x higher levels then horses. This means that in stead of the typical equine range being 1-35 U/L a typically donkey’s range would be up to ~105 U/L. Lucky’s test showed he had 120 U/L which is still elevated but not much. It took sometime to get Luck from the field when the vet arrived- he ran around non stop. The excitement and anxiety could be the cause of the elevated levels.
RBC:
Katherine Wilson, DVM, DACVIM, of the Virginia–Maryland Regional College of Veterinary Medicine (See more at: http://equusmagazine.com/article/decode-horses-bloodwork-27122#sthash.sc4J1ISJ.dpuf) explains “RBC count is probably the least helpful information because horses usually don’t have big changes in red blood cell numbers. It is not uncommon for horses to have an RBC count a little lower than normal range, however. The term we use for low RBC is anemia, but unless the count gets very low, a horse doesn’t necessarily need to be treated for that condition. A lot of diseases or any chronic long-term disease can cause mild anemia. Usually if we see mild anemia on the bloodwork and the horse has other issues, the anemia is just an indication that we need to fix/treat another problem.”
Low or Elevated Values
- Splenic contraction.
- Polycythemia (rare) .
- Dehydration.
- Consider causes of anemia
- Blood loss .
- Hemolysis (i in vivo or artifact).
- Decreased bone marrow production.
- Poor technique at sampling.
- Poor handling and storage of samples.
- Poor technique in laboratory.
Low Bilirubin:
Elevated Hemoglobin (19 g/dL):
According to vetstream.com, Thoroughbred and other “hot-blooded” horses Hemoglobin range differs from other equine- the thoroughbred range = 11.0-19.0g/l.
Elevated Hematocrit (54 %):
Elevated levels could be due to;
- Dehydration.
- Splenic contraction.
- Polycythemia .
“A measurement of the relative amount of red blood cells present in a blood
sample. After blood is drawn, a small tube is filled and centrifuged to separate the heavier
blood cells from the lighter white blood cells and the even lighter fluid (plasma or serum)
portion. A higher than normal reading generally indicates dehydration (same number of
cells in less plasma volume) or may be due to splenic contraction secondary to
excitement or the demands of exercise. A low reading may indicate anemia, though not
invariably. Highly fit athletic horses may normally have a slightly lower hematocrit at
rest due to an overall more efficient cardiovascular system. Evaluation of true anemia in
horses requires several blood samples over a 24-hour period” (Susan Garlinghouse, 2000/ http://www.equinedoc.com/PrideProjectInfo.html).
It took sometime to get Luck from the field when the vet arrived- he ran around non stop. The excitement and anxiety could be the cause of the elevated levels.
Low Sodium:
According to horseprerace.com, “Low levels indicate depletion and are often a predisposing factor, along with dehydration, in fatigue, muscle cramps, colic, synchronous diaphragmatic flutter (“thumps”), diarrhea and other symptoms of exhausted horse syndrome. Even seemingly normal or high-normal levels may in reality be lower, but appear higher due to concentration secondary to dehydration as measured by total protein and albumin levels. Therefore, levels at the lower end of the normal range should be evaluated relative to concurrent dehydration.”
More information on your horse’s blood work
Decoding your horse’s blood work
A Better Understanding of the Results
The vet suggested that I add water to Luck’s and C’s feed in case their values are due to dehydration. She also explained that some of the values may be a result of running around in the field right before drawing them along with anxiety.
The anxiety and running around seemed fair but I am hesitant on the dehydration portion. Yes, I know it is winter and that horses are less likely to drink as much water. But if it were due to dehydration then the Albumin would be low as well. But, the blood work revealed that the Albumin was 2.8 (Luck) and 3.2 (Chance). These values are within the normal range…. that being said, the results could also be due to lab handling especially the Potassium levels.
While speaking with my uncle Jerry (the horse whisperer), he suggested adding a salt block to the horse’s feed. This will increase the horse’s thirst which will get them drinking more. I also added heated water buckets so that the water won’t freeze and in case they are less inclined to drink when the water is cold.
In order to feel comfortable about my horse and donkey being healthy, I will have more blood work done this week to make sure everything is in fact okay.

A Month Later
Luckily, after about one week of stall rest and hand walking, along with a stronger anti-inflammatory, Chance has begun to show improvements over the last couple weeks of treatment.
Chance has almost completed his first 30 days of EPM treatment and has about a day or so left of the Protazil. He is going to continue his other medications and supplements:
1. SmartPak: senior flex and immune boost
2. Vitamin E
3. MicroLactin (amazing) to help with regrowth of his cells, inflammation, and pain.
As I’m doing research, and trying to come up with a plan of action, once again I am inundated with opinions…medication, exercise, holistic, massage, acupuncture, chiropractic, organic, shoeing, etc.
I know I need to continue therapy, or start a new therapy. But which one do I choose?
Do I go the holistic approach and work with an acupuncturist, chiropractor, massage therapist, and vitamins such as Vita Royals? Do I go organic? Or do I try Marquis? Another month of Protazil? Oraquin-10? Rebalance has been linked to a number of recent deaths in the past handful of months. If I go the organic or holistic approach do I run the risk of the disease progressing? If I go with the medication do I run the risk of yet another “treatment crisis”?
I contacted Vet4 and he suggested doing another round of the Protazil or Marquis. I decided on trying Marquis and waited for it to arrive.
Chance after a month on Protazil
Our Regiment
Chance receives the following:
AM:
1. Protazil 50mls
2. Vitamin E 4 scoops (Watch for loose stools. This would indicate that his VitE should be cut down)
PM:
1. SmartPak: Immune Boost
2. SmartPak: Senior Flex
3. Equinyl 2 scoops first two weeks, 1 scoop after
OTHER:
If Chance’s symptoms are worse, he can receive Equinox and UlcerGuard.
CHRONIC PROGRESSIVE LYMPHEDEMA (CPL) due to Scratches
Chance has always been fighting “scratches” on his back legs. Frustrating, painful, and never seem to completely go away. Could scratches have caused this? My thoughts- scratches allowed bacteria to enter the leg, the infection settled on the DDFT sheath and caused the current flare up. Below is some research I found on possible conditions due to scratches that caused similar symptoms Chance had been experiencing.
CHRONIC PROGRESSIVE LYMPHEDEMA (CPL) due to Scratches
A condition characterized by progressive swelling, hyperkeratosis and fibrosis of distal limbs has been characterized in Shires, Clydesdales and Belgian Draft horses and unfortunately affects numerous horses within these breeds. The disease has also been recognized in Gipsy Vanners; however, only a few horses have been evaluated at this point of time. This chronic progressive disease starts at an early age, progresses throughout the life of the horse and often ends in disfigurement and disability of the legs, which inevitably leads to the horse’s premature death. The pathologic changes and clinical signs closely resemble a condition known in humans as chronic lymphedema or elephantiasis nostras verrucosa. The condition has therefore been referred to as chronic progressive lymphedema (CPL). The lower leg swelling is caused by abnormal functioning of the lymphatic system in the skin, which results in chronic lymphedema (swelling), fibrosis, decreased perfusion, a compromised immune system and subsequent secondary infections of the skin.
The clinical signs of this disease are highly variable. It is often first addressed as a marked and “therapy-resistant” pastern dermatitis (scratches). The earliest lesions, however, are characterized by skin thickening, slight crusting and possible skin folds in the pastern area. While readily palpable, these early lesions are often not appreciated visually as the heavy feathering in these breeds covers these areas. Upon clipping of the lower legs, it becomes obvious that the lesions are far more extensive than expected. Secondary infections develop very easily in these horse’s legs and usually consist of chorioptic mange and/or bacterial infections. Pigmented and non-pigmented skin of the lower legs are affected. Appropriate treatment of the infections (pastern dermatitis) is not successful as underlying poor perfusion, lymphedema and hyperkeratosis in association with the heavy feathering present perfect conditions for repetitive infections with both chorioptic mange as well as bacterial infections. Recurrent infections and inflammation will enhance the lymphedema and hence, the condition becomes more chronic. As a result, the lower leg enlargement becomes permanent and the swelling firm on palpation. More thick skin folds and large, poorly defined, firm nodules develop. The nodules may become quite large and often are described as “golf ball” or even “baseball” in size. Both skin folds and nodules first develop in the back of the pastern area. With progression, they may extend and encircle the entire lower leg. The nodules become a mechanical problem because they interfere with free movement and frequently are injured during exercise. This disease often progresses to include massive secondary infections that produce copious amounts of foul-smelling exudates, generalized illness, debilitation and even death.
TREATMENT/MANAGEMENT
Please keep in mind that none of these treatments listed below will “heal” chronic progressive lymphedema (CPL). However, a rigorous management following our suggestions below will assist you to slow down the process and even make some of the nodular lesions disappear. Your horse will need this management the rest of its life.
• Clipping of the feathers
Long and dense feathering makes management of lymphedema more difficult. We highly recommend clipping the feathers and keep them short, if horses are not presented at shows. If you have a show horse, we still recommend to clip the feathers to initiate a rigorous treatment. As the skin condition improves and the edema is reducing – you may have a better chance to keep the horse’s legs in better condition by. careful repetitive treatment, while the feathering is growing back. The feathers are usually back to their original length in about 10-12 months.
• Treatment of skin infections
Progression of lymphedema is also associated with deposition of fibrous tissue and formation of fibrotic nodules.. As a result, these horses have a poor blood circulation and immune response in the skin of their legs. They tend to built up a thick keratin layer. The long feathering further occludes the skin surface, which then remains humid. These factors provide the perfect culture environment for infectious pathogens. This explains why horses with CPL constantly battle recurrent infections with mites (Chorioptic mange) and bacterial infections (Staphylococcus, Dermatophilus).
Horses with CPL should consistently be treated against reinfestation of mites and bacteria:
Topical treatments:
• Careful washing, cleaning and drying of the legs on a routine basis is essential. Horses with long feathering may require blow-drying of their legs. We recommend using a product manufactured by HydroSurge Inc. ( http://www.hydrosurge.com ) called Apricot Sulfur Skin Treatment Shampoo.
• Frontline spray to treat chorioptic mange (do not use Frontline on pregnant and nursing mares)
• The best and most economical topical treatment is to find a source of wettable sulfur powder (“flowers of sulfur”). This can usually be found through a vineyard supply or at your local nursery (certain “rose dust” preparations). Mix this powder with mineral oil in to form a creamy paste. You can mix a moderate amount in a plastic lidded container or glass jar so that you have enough to last 2-4 weeks at a time. Apply this mixture to the ulcerated and/or affected areas of skin daily. This preparation is the best and most economical topical treatment we have found. You can use it indefinitely. Sulfur is safe to use in pregnant mares.
Systemic antiparasitic treatment: Frequent ivermectine treatment will also assist to keep the mites away.
• Exercise
Regular exercise is crucial. It will increase the circulation and the lymph drainage.
• Manual Lymph-drainage
Manual lymph-drainage is regularly used in humans with lymphedema as long as there is no inflammation present within the tissue. MLD has been successfully used in horses with more acute lymphedema, but has not been established yet in horses with progressed CPL. A massaging coldwater stream may assist a massage. It is important to dry the skin before applying anything else after massage and rinsing. If the feathers were not clipped this may take a long time and you may have to use a hair dryer. Your horse may become more compliant to this treatment as swelling reduces over time
• Bandaging and stockings
We have some limited experience with using special bandages developed for people with lymphedema. For horses, which always move around, “short-stretch” bandages should be used (example: Rosidal ®). Short stretch bandages have been successfully used in three horses with clipped feathering; but bandaging was not as successful on horses with long feathers. Of course it is crucial to have very good padding and keeping the bandages fairly tight. If tolerated, the best results will be achieved by keeping the bandages on 24/7. Of course they need to be redone at least every other day – better every day to control the legs. At first, there will be oozing from the lymphedema through the skin – so the bandages will get wet and have to be changed every day. With the reduction of the edema – this will stop. If the horse is only walked quietly the bandages can be left on for the exercise; very likely the legs have to be rewrapped after the exercise as the swelling will somewhat reduce. For more exercise it may be better to take the bandages off, use working bandages and then switch back to the short–stretch bandages after work. Again make sure the skin is dry when you rewrap.
After the edema has been reduced by using bandages – stockings are used for people to maintain avoid recurrence of lympedema. The use of such stockings in horses are currently under investigation.
It should be noted that horses suffering from CPL often are susceptible to reapeated bouts of “Thrush”. Consequently, thorough and routine foot trimming care is an essential part of the health care management for these horses.












