Equine Vaccination Cheat Sheet – The Horse
— Read on thehorse.com/137994/equine-vaccination-cheat-sheet/
Tag Archives: prevention

Three Ways You May Be Inadvertently Putting Your Barn at Risk for Fire
More so than from other tragedies, I find myself physically as well as emotionally affected by these stories. As the horses usually have absolutely no chance of escaping, I think it is probably the horse owner’s worst nightmare.
Emotions aside, in my job as a professional electrician, I am mindful that many of these fires are caused by faulty electrical wiring or fixtures. Over the year,s I have borne witness to my share of potential and actual hazards. Designing a barn’s electrical system to today’s codes and standards is a topic for another day. For today, let’s address what we can do to make the existing horse barn safer.
I can’t cite statistics or studies, but my own experience shows the main safety issues that I am exposed to fall into three general categories:
- Using extension cords in place of permanent wiring
- Exposed lamps in lighting fixtures, and
- Overloading of branch circuits.
The first item I am addressing is extension cords.
I am often asked how extension cords can be UL-listed and sold if they are inherently unsafe. The answer is that cords are not unsafe when used as intended, but become so when used in place of permanent wiring.
The main concern is that most general purpose outlets in barns are powered by 15 or 20 ampere circuits, using 14 or 12 gauge building wiring, respectively. Most cords, however, for reasons of economy and flexibility, are rated for 8 or 10 amperes, and are constructed of 18 or 16 gauge wiring. That’s no problem if you are using the cord as intended—say, powering a clipper that only draws 1 to 4 amperes.
The problem comes when the cord is left in place, maybe tacked up on the rafters for the sake of “neatness.” You use it occasionally, but then winter comes and you plug a couple of bucket heaters into it. When the horses start drinking more water because it’s not ice cold, two buckets become four—or more.
If they draw 2.5 amperes each, you are now drawing 10 amperes on your 18 gauge extension cord that is only rated to carry 8 amperes. The circuit breaker won’t trip because it is protecting the building wiring, which is rated at 20 amperes. A GFCI outlet won’t trip either because the problem is an overload, not a ground fault.
Anyway, next winter, you decide to remove two of the buckets and add a trough outside the stall with a 1500 watt heater, which draws 12.5 amps at 120 volts. If you thought of it, you even replaced the old 18 gauge cord with a 16 gauge one that the package called “heavy duty.” Now the load is 17.5 amperes on a cord that is designed to handle 10 amperes.
In this case, it is possible to overload a “heavy duty” cord by using it at 175% of its rated capacity and never trip a circuit breaker. What has happened is, we’ve begun to think of the extension cord as permanent wiring, rather than as a temporary convenience to extend the appliance cord over to the outlet.
In doing so, we have created an unsafe condition.
Overloaded cords run hot. Heat is the product of too much current flowing over too small a wire. The material they are made of isn’t intended to stand up over time as permanent wiring must. It’s assumed that you will have the opportunity to inspect it as you unroll it before each use.

The second item on our list is exposed lamps (bulbs) in lighting fixtures.
Put simply, they don’t belong in a horse barn. A hot light bulb that gets covered in dust or cobwebs is a hazard. A bulb that explodes due to accumulating moisture, being struck by horse or human, or simply a manufacturing defect introduces the additional risk of a hot filament falling onto a flammable fuel source such as hay or dry shavings.
In the case of an unguarded fluorescent fixture, birds frequently build nests in or above these fixtures due to the heat generated by the ballast transformers within them. Ballasts do burn out, and a fuel source—such as that from birds’ nesting materials—will provide, with oxygen, all the necessary components for a fire that may quickly spread to dry wood framing.
The relatively easy fix is to use totally enclosed, gasketed and guarded light fixtures everywhere in the barn. They are known in the trade as vaporproof fixtures and are completely enclosed so that nothing can enter them, nothing can touch the hot lamp, and no hot parts or gases can escape in the event of failure.
The incandescent versions have a cast metal wiring box, a Pyrex globe covering the lamp, and a cast metal guard over the globe. In the case of the fluorescent fixture, the normal metal fixture pan is surrounded by a sealed fiberglass enclosure with a gasketed lexan cover over the lamps sealed with a gasket and secured in place with multiple pressure clamps.

The last item, overloaded branch circuits, is not typically a problem if the wiring was professionally installed and not subsequently tampered with. If too much load is placed on a circuit that has been properly protected, the result will be only the inconvenience of a tripped circuit breaker.
The problem comes when some “resourceful” individual does a quick fix by installing a larger circuit breaker. The immediate problem, tripping of a circuit breaker, is solved, but the much more serious problem of wiring that is no longer protected at the level for which it was designed, is created.
Any time a wire is allowed to carry more current than it was designed to, there is nothing to stop it from heating up to a level above which is considered acceptable.
Unsafe conditions tend to creep up on us—we don’t set out to create hazardous conditions for our horses.
Some may think it silly that the electrical requirements in horse barns (which are covered by their own separate part of the National Electric Code) are in many ways more stringent than those in our homes.
I believe that it makes perfect sense. The environmental conditions in a horse barn are much more severe than the normal wiring methods found in the home can handle. Most importantly, a human can usually sense and react to the warning signals of a smoke alarm, the smell of smoke, or of burning building materials and take appropriate action to protect or evacuate the occupants. Our horses, however, depend on us for that, so we need to use extra-safe practices to keep them secure.
As I always state in closing my electrical safety discussions, I know that we all love our animals. Sometimes in the interest of expedience, we can inadvertently cause conditions that we never intended. Electrical safety is just another aspect of stable management. I often use the words of George Morris to summarize:
“Love means giving something our attention, which means taking care of that which we love. We call this stable management.”
About the Author
Thomas Gumbrecht began riding at age 45 and eventually was a competitor in lower level eventing and jumpers. Now a small farm owner, he spends his time working with his APHA eventer DannyBoy, his OTTB mare Lola, training her for a second career, and teaching his grandson about the joy of horses. He enjoys writing to share some of life’s breakthroughs toward which his horses have guided him.

Immune Booster Leads to Infection?
For the past 6 weeks, my horse has been receiving Ozonetherapy to aid in his chronic back leg related issues- dermatitis (“scratches”), previous DDFT tendon laceration, a history of Lymphingitis, and the residual scar tissue from his DDFT injury. Due to his age (27), he lacks proper circulation in his hind end which does not help him fight his pastern dermatitis.
According to the American Academy of Ozonetherapy, Ozonetherapy is described as;
“Ozonotherapy is the use of medical grade ozone, a highly reactive form of pure oxygen, to create a curative response in the body. The body has the potential to renew and regenerate itself. When it becomes sick it is because this potential has been blocked. The reactive properties of ozone stimulate the body to remove many of these impediments thus allowing the body to do what it does best – heal itself.”
“Ozonotherapy has been and continues to be used in European clinics and hospitals for over fifty years. It was even used here in the United States in a limited capacity in the early part of the 20th century. There are professional medical ozonotherapy societies in over ten countries worldwide. Recently, the International Scientific Committee on Ozonotherapy (ISCO3) was formed to help establish standardized scientific principles for ozonotherapy. The president of the AAO, Frank Shallenberger, MD is a founding member of the ISCO3.”
“Ozonotherapy was introduced into the United States in the early 80’s, and has been increasingly used in recent decades. It has been found useful in various diseases;
- It activates the immune system in infectious diseases.
- It improves the cellular utilization of oxygen that reduces ischemia in cardiovascular diseases, and in many of the infirmities of aging.
- It causes the release of growth factors that stimulate damaged joints and degenerative discs to regenerate.
- It can dramatically reduce or even eliminate many cases of chronic pain through its action on pain receptors.
- Published papers have demonstrated its healing effects on interstitial cystitis, chronic hepatitis, herpes infections, dental infections, diabetes, and macular degeneration.”
After doing research and speaking to one of my good friends, we determined that Chance’s flare up of Lymphingitis, after almost 3 years of not a single issue, could possibly be caused by his immune system’s response to Ozonetherapy. Let me explain.
Chance suffers from persistent Pastern dermatitis (“scratches”) since I purchased him in 2000. I have tried everything- antibiotics, every cream and ointment and spray for scratches, diaper rash ointment, iodine and vaseline mix, Swat, laser treatments, scrubs and shampoos, shaving the area, wrapping the area, light therapy…you name it, I have tried it. So, when we began Ozonetherapy to help break down the left over scar tissue from his old DDFT injury, I noticed that his scratches were drying up and falling off. We continued administering the Ozonetherapy once a week for about 6 weeks. The improvement was dramatic!
However, one day Chance woke up with severe swelling in his left hind leg and obviously, he had difficulty walking. He received Prevacox and was stall bound for 24 hours. The vet was called and she arranged to come out the following day. The next morning, Chance’s left leg was still huge and he was having trouble putting weight on it. I did the typical leg treatments- icing, wrapping. The swelling remained. I tried to get him out of his stall to cold hose his leg and give him a bath but he would not budge. He was sweaty and breathing heavily and intermittently shivering. So, I gave him an alcohol and water sponge bath and continued to ice his back legs. I sat with him for 4 hours waiting for the vet to arrive. He had a fever and wasn’t interested in eating and his gut sounds were not as audible. He was drinking, going to the bathroom, and engaging with me. I debated giving him Banamine but did not want it to mask anything when the vet did arrive.
The vet arrived, gave him a shot of Banamine and an antihistamine and confirmed that Chance had a fever of 102 degrees and had Lymphingitis. There was no visible abrasion, puncture, or lump… I asked the vet to do x-rays to ensure that he did not have a break in his leg. The x-rays confirmed that there was no break. The vet suggested a regiment of antibiotics, steroids (I really am against using steroids due to the short-term and long-term side effects but in this case, I would try anything to make sure he was comfortable) , prevacox, and a antacid to protect Chance from stomach related issues from the medications. It was also advised to continue to cold hose or ice and keep his legs wrapped and Chance stall bound.
The following day, Chance’s legs were still swollen but his fever had broken. The vet called to say that the CBC had come back and that his WBC was about 14,00o. She suggested that we stop the steroids and do the antibiotic 2x a day and add in Banamine. I asked her if she could order Baytril (a strong antibiotic that Chance has responded well to in the past) just in case. And that is what we did.
Being as Chance had such a strong reaction to whatever it was, I did some thinking, discussing, and researching…first and foremost, why did Chance have such an extreme flare up of Lymphingitis when he was the healthiest he has ever been? And especially since he had not had a flare up in 3+ years…plus, his scratches were getting better not worse. The Ozonetherapy boosted his immune system and should provide him with a stronger defense against bacteria, virus’, etc. So why exactly was he having a flare up? And that is when it hit me!
In the past when Chance began his regiment of Transfer Factor (an all natural immune booster), he broke out in hives. The vet had come out and she felt it was due to the Transfer Factor causing his immune system to become “too strong” and so it began fighting without there being anything to fight, thus the hives. My theory- Chance started the Ozonetherapy and his body began to fight off the scratches by boosting his immune system. As the treatments continued, his immune system began to attack the scratches tenfold. This resulted in his Lymphatic system to respond, his WBC to increase, and his body temperature to spike. Makes sense…but what can I do to ensure this is not going to happen again?
My friend suggested attacking the antibiotic resistant bacteria by out smarting them…okay, that seems simple enough…we researched the optimal enviroments for the 3 types of bacteria present where Chance’s scratches are (shown in the results of a past skin scape test). The bacteria – E. Coli, pseudomonas aeruginosa and providencia Rettgeri. The literature stated that PA was commonly found in individuals with diabetes…diabetes…SUGAR! How much sugar was in Chance’s feed? I looked and Nutrina Safe Choice Senior feed is low in sugar…so that is not it. What else can we find out? The optimal temperature for all three bacteria is around 37 degrees celsius (or 98.6 degrees fahrenheit), with a pH of 7.0, and a wet environment. Okay, so, a pH of 7.0 is a neutral. Which means if the external enviroment (the hind legs)pH is thrown off, either to an acidic or alkaline pH, the bacteria will not have the optimal enviroment to continue growing and multiplying. How can I change the pH?
Vinegar! An antimicrobial and a 5% acetic acid! And…vinegar is shown to help kill mycobacteria such as drug-resistant tuberculosis and an effective way to clean produce; it is considered the fastest, safest, and more effective than the use of antibacterial soap. Legend even says that in France during the Black Plague, four thieves were able to rob the homes of those sick with the plague and not become infected. They were said to have purchased a potion made of garlic soaked in vinegar which protected them. Variants of the recipe, now called “Four Thieves Vinegar” has continued to be passed down and used for hundreds of years (Hunter, R., 1894).
I went to the store, purchased distilled vinegar and a spray bottle and headed to the farm. I cleaned his scratches and sprayed the infected areas with vinegar. I am excited to see whether our hypothesis is correct or not…I will keep you posted!
References & Information
Effect of pH on Drug Resistent Bacteriaijs-43-1-174
What does my horse’s CBC mean?

Nutrena SC Senior feed ingredience
The American Academy of Ozonetherapy
Hunter, Robert (1894). The Encyclopaedic Dictionary. Toronto: T.J. Ford. ISBN 0-665-85186-3.

How To Read Equine (Horse and donkey) Blood Work?
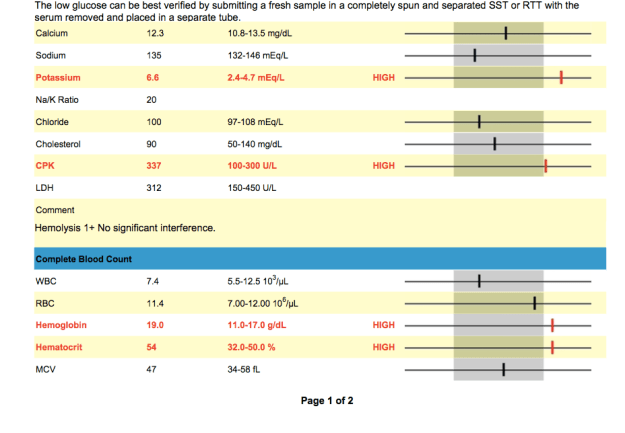
I had the vet run some blood work on Luck and Chance as a precaution, because of the “Panic Grass” in Virginia has been causing liver failure in horses, and because I like to do a full work up every 6-12 months.
Chance’s Blood Work



INTERPRETATION OF RESULTS
Elevated Potassium (6.6 mEq/L):
Low Sodium:
“Low levels commonly indicate loss through excessive sweating, or through kidney or intestinal disease. Low levels may also be found in young foals with bladder damage. Increased sodium levels are usually a sign of dehydration” (http://www.minstervets.co.uk).
Low Platelets:
This was the most worrisome in regards to the potential immediate issues that could ensue because of the low platelet count.
Low Glucose:
“Glucose is the source of the body’s energy. It is measured in suspected cases of equine metabolic syndrome and sometimes in cases of equine Cushing’s disease. Blood glucose may also be measured as part of a glucose tolerance test, assessing small intestinal function” (http://www.minstervets.co.uk).
Levels 2-3x the highest number in range are considered significant according to vetstream.com. Levels are easily increased due to poor handling techniques as well as lab error.
According to Dr. Christine Woodford and Carla Baumgartner on vipsvet.com, “Elevations of CPK and SGOT are indictors of muscle inflammation–tying-up or rhabdomyolysis. The term “rhabdo” means muscle and “myolysis” means rupture of muscle cells. The CPK and SGOT are very sensitive indicators of skeletal muscle damage, and they rise in concentration proportionally with the amount of damage. A bit of timing is required in order to obtain the most sensitive results; CPK rises (due to its leakage from muscle cells into the blood system) approximately six to eight hours after the onset of muscle inflammation, and SGOT rises after approximately 12-14 hours. The absolute peak of CPK concentration and the time it takes to return to normal are important indicators of the severity of muscle damage and the response to therapy.”
Elevated MCV: Is the average volume of red blood cells.
- Macrocytosis.
- Indicates immature RBC in circulation (suggests regenerative anemia).
- Very rare in the horse, but may observe increasing MCV within normal range as horses increase erythropoiesis.
According to Vetstream.com, “Macrocytosis (increased MCV) resulting from release of immature RBC from the bone marrow during regeneration is very rare in the horse therefore the MCV is less useful in the horse than in other species.”
Elevated MCH: Is the average amount of hemoglobin in an individual red blood cell.
- Hemolysis, if intravascular in nature .
- Errors can occur during processing
Low RBC:
Luck’s blood work

Elevated Potassium: Potassium can become elevated for a number of reasons.
According to Vetstream.com,
- 98% of potassium is intracellular.
- Changes in serum or plasma potassium levels reflect fluid balance, rate of renal excretion and changes in balance between intra- and extracellular fluid.
- Hypokalemia increases membrane potential, resulting in hyperpolarization with weakness or paralysis.
- Hyperkalemia decreases membrane potential with resulting hyperexcitability.
- Results can be false due to processing time (ie: if the lab waited too long to process blood sample)
- Immediately after high intensity exercise.
- In association with clinical signs in horses with hyperkalemic periodic paraysis (HYPP) .
- Bladder rupture (neonate) .
- Hypoadrenocorticism [Pituitary: adenoma] (rare).
- Metabolic acidosis.
- Acute renal failure .
- Extensive tissue damage (especially muscle).
- IV potassium salts, eg potassium benzyl penicillin, potassium chloride .
- Phacochromocytoma (rare in the horse).
Hypokalemia - Chronic diarrhea.
- Diuretic therapy, especially potassium-losing diuretics.
- Excess bicarbonate/lactate therapy.
- Chronic liver disease .
- Acute renal failure (polyuric phase) .
- Recovery from severe trauma.
- Metabolic/respiratory alkalosis.
- Prolonged anorexia.
- Recovery period after high intensity exercise (30-60 min after).
- Parenteral feeding.
In combination with clinical signs and results of other tests results could signify the following;
- Muscle injury .
- Acute renal failure .
- Diarrhea.
- Tissue injury.
- Acid-base balance.
Elevated GGTP:
* Donkeys tend to have 3x higher levels then horses. This means that in stead of the typical equine range being 1-35 U/L a typically donkey’s range would be up to ~105 U/L. Lucky’s test showed he had 120 U/L which is still elevated but not much. It took sometime to get Luck from the field when the vet arrived- he ran around non stop. The excitement and anxiety could be the cause of the elevated levels.
RBC:
Katherine Wilson, DVM, DACVIM, of the Virginia–Maryland Regional College of Veterinary Medicine (See more at: http://equusmagazine.com/article/decode-horses-bloodwork-27122#sthash.sc4J1ISJ.dpuf) explains “RBC count is probably the least helpful information because horses usually don’t have big changes in red blood cell numbers. It is not uncommon for horses to have an RBC count a little lower than normal range, however. The term we use for low RBC is anemia, but unless the count gets very low, a horse doesn’t necessarily need to be treated for that condition. A lot of diseases or any chronic long-term disease can cause mild anemia. Usually if we see mild anemia on the bloodwork and the horse has other issues, the anemia is just an indication that we need to fix/treat another problem.”
Low or Elevated Values
- Splenic contraction.
- Polycythemia (rare) .
- Dehydration.
- Consider causes of anemia
- Blood loss .
- Hemolysis (i in vivo or artifact).
- Decreased bone marrow production.
- Poor technique at sampling.
- Poor handling and storage of samples.
- Poor technique in laboratory.
Low Bilirubin:
Elevated Hemoglobin (19 g/dL):
According to vetstream.com, Thoroughbred and other “hot-blooded” horses Hemoglobin range differs from other equine- the thoroughbred range = 11.0-19.0g/l.
Elevated Hematocrit (54 %):
Elevated levels could be due to;
- Dehydration.
- Splenic contraction.
- Polycythemia .
“A measurement of the relative amount of red blood cells present in a blood
sample. After blood is drawn, a small tube is filled and centrifuged to separate the heavier
blood cells from the lighter white blood cells and the even lighter fluid (plasma or serum)
portion. A higher than normal reading generally indicates dehydration (same number of
cells in less plasma volume) or may be due to splenic contraction secondary to
excitement or the demands of exercise. A low reading may indicate anemia, though not
invariably. Highly fit athletic horses may normally have a slightly lower hematocrit at
rest due to an overall more efficient cardiovascular system. Evaluation of true anemia in
horses requires several blood samples over a 24-hour period” (Susan Garlinghouse, 2000/ http://www.equinedoc.com/PrideProjectInfo.html).
It took sometime to get Luck from the field when the vet arrived- he ran around non stop. The excitement and anxiety could be the cause of the elevated levels.
Low Sodium:
According to horseprerace.com, “Low levels indicate depletion and are often a predisposing factor, along with dehydration, in fatigue, muscle cramps, colic, synchronous diaphragmatic flutter (“thumps”), diarrhea and other symptoms of exhausted horse syndrome. Even seemingly normal or high-normal levels may in reality be lower, but appear higher due to concentration secondary to dehydration as measured by total protein and albumin levels. Therefore, levels at the lower end of the normal range should be evaluated relative to concurrent dehydration.”
More information on your horse’s blood work
Decoding your horse’s blood work
A Better Understanding of the Results
The vet suggested that I add water to Luck’s and C’s feed in case their values are due to dehydration. She also explained that some of the values may be a result of running around in the field right before drawing them along with anxiety.
The anxiety and running around seemed fair but I am hesitant on the dehydration portion. Yes, I know it is winter and that horses are less likely to drink as much water. But if it were due to dehydration then the Albumin would be low as well. But, the blood work revealed that the Albumin was 2.8 (Luck) and 3.2 (Chance). These values are within the normal range…. that being said, the results could also be due to lab handling especially the Potassium levels.
While speaking with my uncle Jerry (the horse whisperer), he suggested adding a salt block to the horse’s feed. This will increase the horse’s thirst which will get them drinking more. I also added heated water buckets so that the water won’t freeze and in case they are less inclined to drink when the water is cold.
In order to feel comfortable about my horse and donkey being healthy, I will have more blood work done this week to make sure everything is in fact okay.

The Best Horse “Hello”
“I Guess I’ll Eat Some Worms…”
It was time for me to deworm my guys and I misplaced my “schedule”, so I decided to go online and print one. Bad idea! There are so many deworming schedules out there…it is easy to get overwhelmed.
I found a deworming quiz that was incredibly helpful when deciding what schedule and dewormers are right for my horse. The quiz & the below information was written by Karen Hayes (an Idaho-based equine practitioner) and was published in the June 1999 issue of Horse & Rider magazine. –
See more at: http://www.equisearch.com/artic/eqdeworm321#sthash.7cTzzRGc.dpuf
Here’s a general program to fight these parasites, but check with your vet to develop a program right for your horse and your particular area.
Bots. Ivermectin and moxidectin are the only available products effective against bots. In a purge deworming program, you can kill two birds with one stone by using one of these products on your regular late-fall and spring treatment dates. Time of year is critical, because fall’s’ first frost kills bot flies, giving you a leg up on reducing their population-especially if you follow up in the spring. Here’s what to do: After first frost, remove/kill any remaining bot eggs or larvae on your horse’s legs with a bot block or knife. Then use a purge dewormer to get rid of adult bots in his system. In spring, remove/kill any external eggs or larvae you may’ve missed in the fall, and deworm him again to zap any adult bots in his stomach before they lay eggs. Then you’ll start bot season (spring through early fall) with a clean slate.
If your horse is on a daily program, give him a dose of ivermectin or moxidectin in early spring and again in late fall, in addition to the daily dewormer.
Tapeworms. Some investigators believe daily deworming effectively controls tapeworms, but the evidence is conflicting. As an extra measure, you have three options:
You can use options one or two to replace your horse’s regular deworming treatments in spring and fall. Give Droncit in addition to the regular deworming treatment, but on a different day, to avoid possible drug interactions.
Encysted cyathostomes. Prevent encysted cyathostomes by putting your horse on a daily deworming program, or kill them by:
Daily verses Purge Programs
For daily programs, it’s critical that your horse gets his daily dose daily, as missed doses will decrease the levels of dewormer in his system, rendering it less effective- See more at: http://www.equisearch.com/article/eqdeworm321#sthash.7cTzzRGc.dp
For purge programs, timing is key. If you treat too early, targeted worms will be too immature to be affected by the dewormer. If you treat too late, adult worms will have the opportunity to produce eggs, infesting your horse’s environment and raising his (and other horses’) risk of exposure.
I hope the information was as helpful for you as it has been for me. For more information on worming and a comparison of the products available click the link below.
Check-Ups
Chance had a chiropractic adjustment, acupuncture, and electro stimulation on his cervical spine. He actually fell asleep resting his head on someone’s shoulder while receiving the stim for 20 minutes.
I also spoke to the vet about Chance’s unrelenting scratches on his hind legs. She suggested mixing Vaseline and Betadine and applying it to the affected area, wrapping seren wrap around it, and then wrapping it with a standing wrap. After 12 hours, remove the wraps and clean area. – scratches not improving. Once scabs have all fallen off then he can begin an Antibiotic like Baytril.
Chance is still stiff on both sides of neck, although he can bend with better balance (when vet holds one of Chance’s front legs up while he bends to the opposite side). He also shows Improved lateral flexibility on right side. Right base dorsal secrum and d-v flexion improved.

Chance’s skin is having a “typical chestnut reaction” and the vet advices to discontinue transfer factor due to his immune system working too hard, and then use 1/2 of current dose. Start Tellurium 1 teaspoon a day for 5 days and then 1x a week to help with his skin.

Chance in heaven while receiving stim
Transfer Factor: An Answer To Treatment and Prevention of Equine Disease?
August 31, 2013
by Heather Smith Thomas
For many decades, the typical way veterinarians and horse owners have dealt with disease is by vaccination and by treating sick animals with anti-microbial drugs when signs of illness appear.
By the time the animal shows symptoms, however, damage has already occurred and it can be more difficult to treat the disease. In some instances, irreversible damage has already been done. The use of pathogen-killing drugs is not always as effective as we’d like, and today this use is also being questioned due to the increasing development of drug-resistant pathogens. This microbial resistance diminishes the effectiveness and benefit of some of the drugs we’ve come to rely on.
Horse owners are beginning to look at alternatives to antimicrobial use in dealing with disease. A bright spot in this quest is the use of immune system enhancement and the role of transfer factors. If the immune status of our animals could be enhanced, disease would be less likely to occur, and even if the animals do get sick, the severity and duration of disease could be reduced and they would recover quicker without the need for as much antimicrobial treatment.
Dr. Steve Slagle, a veterinarian in Granite Bay, California, near Sacramento, has been working with a fascinating product that is now available for humans and animals. “The product that I’m using in my practice is a natural immune enhancer and modulator. It derives its efficacy from a protein produced by the immune system’s master immune cells called T lymphocytes. The protein is called transfer factor, and it is also found in cow colostrum. If you buy a bag of dried colostrum (a substitute colostrum product for newborn calves) at the feed store or veterinary supply, about 1% of that product is this protein. We extract that 1% from cow colostrum which enables us to deliver very high levels of transfer factor in our products,” he explains.
“The transfer factors were originally marketed as a human product. I started using them in my veterinary practice in February 1999. So many veterinarians were using the human product that 4Life Research decided to create a veterinary product line for dogs, cats, horses and newborn livestock. Dr. Joe Ramaekers, a colleague of mine, was asked to formulate the product line. Dr. Ramaekers then went on to develop a cancer product for dogs and cats, and a formulation for ruminating livestock,” says Slagle.
“I have been practicing veterinary medicine since 1968 and I have never seen anything that is as exciting as this. I must admit that when I was first informed about transfer factor by a longtime friend, a small animal veterinarian, I was skeptical. He claimed success on so many different types of cases. This didn’t really make sense or seem feasible until I realized some time later that the transfer factors were not treating the particular condition. They were simply enabling the immune system to do its job,” says Slagle
“During the first month I tried it, I used transfer factor on three foals. All three cases were critical and I felt their chances for recovery were slim. The first one was a severe pneumonia. The second was a joint ill infection involving the hock. The third was a terminal septicemia. All three made dramatic recoveries, so I was more than impressed. I was amazed,” he says.
EQUINE PRODUCTS
“The two products from 4Life Research that I use most often in my equine practice are Equine Performance & Show (patented for tumors, EPM, Cushing’s and several other diseases) and Animal Stress Pack (for treating acute conditions). Equine Performance & Show is used primarily as a complete high-end daily supplement with maintenance levels of transfer factor and other immune-enhancing ingredients. I also use it on my chronic cases like tumors, Cushing’s, allergies, and autoimmune diseases like pemphigus (a chronic skin disease). Animal Stress Pack is my emergency treatment, with high levels of transfer factor and other immune enhancers, probiotics, electrolytes and stress vitamins,” says Slagle.
“One of our first studies in horses was done at a major Quarter Horse ranch in Texas that was fighting a losing battle against strangles and a rhodococcus outbreak in which they had already lost several very valuable foals. We put the remaining affected foals on Animal Stress Pack and turned the tide on this very serious situation. All of my infectious disease cases receive the Stress Pack. Even though it is not treating any particular disease, we are dramatically improving the immune response, giving the immune system—which is the ultimate disease fighter—the tools it needs to finish the job,” he explains.
This product is patented for use in horses with EPM. At the latest AAEP Convention in Anaheim, California, Slagle met with Dr. Thomas Bello (a research veterinarian with a private practice, Sandhill Equine Center, in North Carolina). Bello had earlier done the clinical trials for a major drug company on their product for treating EPM.
“The literature on EPM treatments had shown that only between 10% to 20% of horses experience full recovery, returning to their original performance levels. Dr. Bello then became interested in our product and began using it for treating horses with EPM, and getting great results,” says Slagle.
“Dr. Bello then presented a paper at the AVMA convention, which was later published in the Journal of Equine Veterinary Science in 2008—showing that 28 performance horses with EPM were treated with the new EPM product along with the two transfer factor products. At the time of publishing, 82% of those horses were in full recovery. In our recent conversation at the AAEP convention, Dr. Bello told me he now has more than 50 cases in the study, and a recovery rate of over 90%. Apparently the additional immune support was what was needed to bring full recovery. It is also very common to see a relapse in horses that are only being treated with antimicrobials, but Dr. Bello indicated that with his regimen he has not experienced this problem,” says Slagle.
“Since transfer factors are true modulators, my allergic and autoimmune patients go on a daily regimen of transfer factor. Somehow this protein is able to re-educate a confused immune system and bring relief to a large percentage of my equine patients. I generally start them on Performance & Show, along with a week or two of the Stress Pack to front-load the system with high levels of transfer factor. Then when symptoms are under control, we continue with only the Performance & Show,” he explains.
The immune system provides the body with the ability to recognize and remember harmful invaders (pathogenic bacteria, viruses and fungi). Suppressed or damaged immune systems can have disastrous results. One of the most devastating examples is SCID (a genetic defect that occurs in some Arabian foals). They are born without a functioning immune system. After the temporary immunity from the dam’s colostrum is gone, these foals always die of disease.
A healthy immune system has the ability to remember and recognize pathogens, mounting a defense against them. Disease occurs in humans and animals when the immune system is overwhelmed by the pathogen.
HOW IT WORKS
The body’s immune system produces memory molecules whenever it is exposed to disease or receives a vaccination. These memory molecules are bioactive peptides. An example is the “immune” factor passed from a mare to her foal or a cow to her calf via colostrum. This transfer is critical in helping the immune response cells (antibodies) with identification and activation. They are what we might call super boosters in immunity.
Transfer factors were discovered in 1949. Earlier, it had been noticed that immunities could be transferred from one person to another by blood transfusions. In 1949, Dr. H. Sherwood Lawrence, a researcher working on the problem of tuberculosis in humans, found that he could transfer immunity to his patients by using dialyzed leukocytes. When this extract was taken from a blood donor who was resistant to the pathogen and injected into a patient that had no immunity, the immunity of the donor was transferred to the naïve patient. A portion of the lymphocyte (white blood cell) contained what Lawrence dubbed “transfer factor”.
Research was conducted in more than 60 countries (and more than 3500 studies were done) during the 1950s through 1970s and then practically halted. At that point in time, the world’s blood supply was becoming contaminated by HIV and hepatitis C virus and the only known source of transfer factor was blood. Research on this phenomenon was also put on hold because more exciting discoveries revolved around antimicrobial drugs. These were the promising wave of the future that could halt diseases in their tracks. Use of transfer factor was very limited for awhile—especially in veterinary medicine—because it was more expensive to produce than antibiotics. Research did continue, but slowly.
The phenomenon of transfer factor was not actively pursued until the late 1980s when it was discovered that bovine colostrum contains significant amounts of this ingredient that stimulates both aspects of the immune system (humoral and cellular immunity). Veterinary researchers observed a large number of lymphocytic cells in the normal mammary gland secretions of cows, and wondered what role they might play in the health of the newborn calf, realizing that colostrum does more than merely provide passive immune protection. We now know that transfer factor is a lymphokine—one of the protein messengers released by antigen-sensitized lymphocytes (white blood cells).
Chicken eggs also contain transfer factors, and the combination derived from eggs and colostrum increases the effectiveness by 185%. Transfer factors from cow colostrum and eggs are superior to and more functional than transfer factors from humans because animals are exposed to many more species and types of bacteria, viruses and fungi.
As stated by Dr. Richard H. Bennett (Infectious Disease Microbiologist and Immunologist, and former consultant to the National Research Council), transfer factor is one of the most potent messengers in the body and has three effects on the immune system. These are called inducer fractions, antigen specific fractions, and suppressor fractions.
Inducer fractions – One of the functions of transfer factor molecules is to selectively enhance immune surveillance by helping the body recognize various antigens. This selective immune surveillance is made possible by the inducer fractions. One of the veterinarians who consulted with the company that has the patent for extracting transfer factor from colostrum stated that one capsule (200 mg) of transfer factor has the capability of recognizing more than 100,000 different pathogens. Not only can transfer factor be specific for an individual antigen that a lymphocyte might be exposed to, but it can also stimulate a multiple response and provide protection against several strains of that organism.
This enhancement is made possible by the inducer fraction that acts on what are called the Natural Killer (NK) Cells, according to Bennett. The NK cell’s job is to seek out any cells that have been altered by microbes and destroy them. They have a similar protective role in preventing the formation of malignant tumors. The inducer fractions also influence the body’s overall response by increasing the function of the T helper lymphocytes which play a critical role in a balanced immune response to resolve most infections, says Bennett.
The researchers found that they could expose the cow to various bacteria and viruses, and the cow would then produce transfer factor that could stimulate immunity not only to those pathogens but also to other related strains that are much more pathogenic to other species. This is of benefit when using transfer factor to aid disease resistance in horses, for instance. Cows can produce large quantities of colostrum that can then be used for extracting transfer factor that can benefit other species—since transfer factor in horses, cats, dogs, humans and cows has similar structure and identical function.
Another exciting aspect of transfer factor is how quickly the protection is mounted. Immunity from vaccination generally takes 10 to 14 days to develop, whereas transfer factor activates immunity in less than 24 hours.
Antigen specific fractions – Transfer factors act in two ways to “educate” the immune system to respond quickly when confronted by disease threat. One is a response to a specific pathogen such as a cryptosporidium protozoan that might be common to several species, and the other response is to similar pathogens—such as herpes virus infections that differ from one host species to another. Thus transfer factors can “educate” the immune system to recognize and fight a wide array of related, but not identical, infectious agents, according to Bennett.
Suppressor fractions – In every physiological system in the body there are checks and balances, so transfer factor can also act to suppress immune function when necessary. The process of achieving balance is called homeostasis. Once a disease threat has been confronted, and a sufficient response has occurred to thwart it, the body must down-regulate the battle so the immune system can return to a resting state and conserve its resources for the next challenge.
The suppressor fractions signal the T helper lymphocytes and the cytotoxic T cells to slow down their activity and return to a quieter state. This “quieting down” the immune response is important because some pathogenic microbes can hide in certain body tissues and the immune response becomes directed toward those tissues, leading to autoimmune diseases. The suppressor fractions of transfer factor appear to be the way the body limits overzealous immune responses, according to Bennett, and becomes the body’s means to protect itself from an inappropriate immune response.
It seems paradoxical that the transfer factor can both stimulate and suppress immune function, but this is part of its important role. Thus it can prevent autoimmune diseases, and other situations where the body’s own immune response has over-responded to antigens, such as allergic reactions and COPD.
HEALTHIER HORSES
Stressed animals generally become more vulnerable to disease because stress (and the resultant rise in cortisol levels) hinders the immune system. Slagle and Ramaekers tested the transfer factor product on stressed calves to see if it controlled cortisol levels. “We have done two controlled studies on stress and cortisol levels of stressed calves entering the feedlot. One was in Tiffin, Ohio at a private, veterinary-owned and operated feedlot. We repeated that study at Texas A&M. Our results were basically the same. We took blood samples twice daily for 12 days and saw a 46% reduction in cortisol levels in the calves that received transfer factor, with a large decrease in treatments, along with better weight gains,” says Slagle.
“We have not repeated that kind of study in horses, but with the responses (reduced incidence of disease in stress situations) we see in horses, I feel the results would be similar,” he says.
The use of transfer factor to stimulate the body to mount a better immune response to pathogens can reduce the need for antimicrobial drugs. This can help retain their effectiveness longer, since over-use of these drugs has led to increasing numbers of resistant pathogens. We need to find ways to maintain their effectiveness as long as possible.
Transfer factor can boost immunity within a few hours. This makes it very beneficial for use in newborn foals, horses that will be transported, or even as a post-exposure treatment when you know a horse has come into contact with disease agents. Veterinarians have also been using transfer factor to help horses deal with frustrating problems like Cushing’s, laminitis, colitis, cancers, allergies, chronic metritis, EPM, pigeon fever, scours, strangles, and many viral diseases. Helping the immune system help itself is the promising wave of the future.
For more information, Dr. Steve Slagle can be reached in Granite Bay, California at 916-791-2911 or Dr. Joe Ramaekers at 831-476-5050 or check his website: www.ramaekersnutrition.com
